authors: Saagar S. Kulkarni,1 Rohan S. Kulkarni,2 MBBS, Kathryn E. Lorenz,3 MD
1 Boonshoft School of Medicine, Wright State University, Dayton, Ohio, USA
2 Dr. DY Patil Medical College, Dr. D Y. Patil Vidyapeeth, Pimpri, Pune, India
3 Clinical Faculty, Boonshoft School of Medicine, Wright State University, Dayton, Ohio, USA
Abstract
As of August 2021 with over 1.6M combined deaths, USA, India, and Brazil had the highest number of COVID-19 infections. This paper examines the populations of the USA and India, with a combined 70M infections and counting, to provide a comprehensive overview and explore the social implications of COVID-19.
For the US, our multivariable regression model was statistically significant between COVID-19 deaths and age/race/residence-states. The trends in age and residence states were significant while the trend for gender was not. However, individual’s age and residence state played a significant role in determining life or death. Socio-economic analysis confirmed the Qualitative socio-economic Logic based Cascade Hypotheses (QLCH) of education/occupation/income affecting race/ethnicity differently. For a given race/ethnicity, education drives occupation then income, where a person lives, and in turn his/her access to healthcare coverage. Considering the QLCH framework, different races are poised for differing effects of COVID-19; specifically, Asians/Whites are in a stronger position to combat COVID-19 compared to Hispanics/Blacks.
For India, the residence-states were found to be statistically significant in a regression of nationality/residence states/and counts for total cases/deaths/and cured. A logistics regression model analyzing age/gender/nationality/and residence states was also statistically significant. Both sexes were affected equally by the virus while age/residence states played important roles in life/death. Higher urban populated states with higher GDP creation had the highest virus related deaths, explaining the forced avoidance of social distancing effect.
1. Introduction
In 2017, the US experienced more than 2.8M deaths due to various causes [1]. Diseases of the heart were the number one cause with a count over 647,000. India in 2019 experienced 10M deaths. By August 2020, due to the virus, the US saw 175,000+ deaths while India experienced 75,000+ deaths [1-2].
Ethnicity likely contributes to the spread of the virus in a community; cultural, behavioral, work and living differences due to socio-economic status, and health-seeking behavior could all contribute [3]. Rentsch et al. found that Blacks/Hispanics veterans tested positive for COVID-19 at a higher rate than Caucasians [4]. Large US metropolitan areas (e.g. Chicago and Milwaukee), with higher concentrations of racial minorities and adverse social determinants, showed a higher rate of COVID-19 infections [5, 6].
For India, Acharya et al. computed the state’s composite index of vulnerability based on domains of socioeconomic, demographic, housing, and hygiene. They observed similarities between vulnerability and concentration of COVID-19 cases at the state level [7]. Kamath et al. list multiple challenges India faces for combating COVID-19, including being densely populated with a huge population, and millions having no access to clean water [8].
This paper specifically looks at demographic factors of age/race/gender/residence-states to find out which demographic factors contribute most to COVID-19 deaths.
2. Data acquisition and analysis
2.1. Database selection
We used data collected by the CDC for the US analyses, limiting our dataset to the first eight months of 2020 including age/race/and residence-states with respect to COVID-19 deaths [9, 19 ]. Our second analysis also included gender [10]. We used Kaggle data for both India population analyses, limiting to COVID-19 deaths for the first eight months for 2020 [11-12]. The first data set included nationality/residence-states/and counts for the total cases/deaths/cured [11]. The second data set included factors of age/gender/nationality/residence-states/status of cured/hospitalized/dead [12].
2.2. Hypothesis testing
Statistical analyses of multiple regression and nominal logistics regression were performed with α = 0.05.
2.3. USA analysis
A visual display in Figure 1 demonstrates that Caucasians have experienced more variation of deaths followed by African Americans, Hispanics, and then Asians.
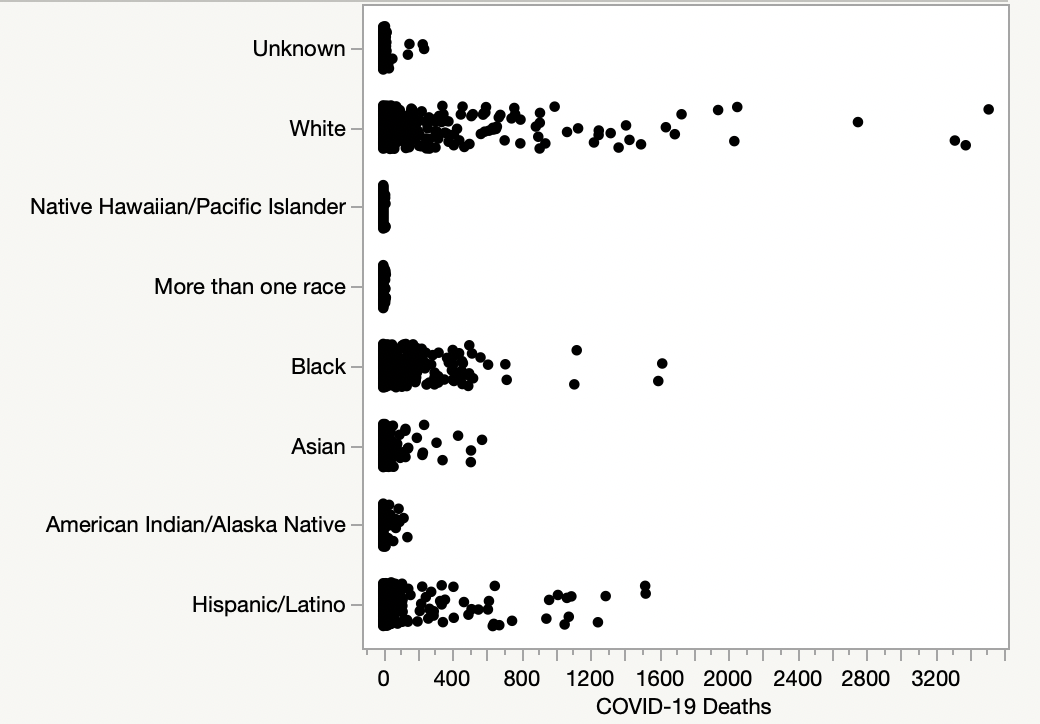
Figure 1. Race-deaths scatterplot
Figure 2 demonstrates an increase in the number of deaths versus age, and that individuals<55 have a relatively smaller chance of death.
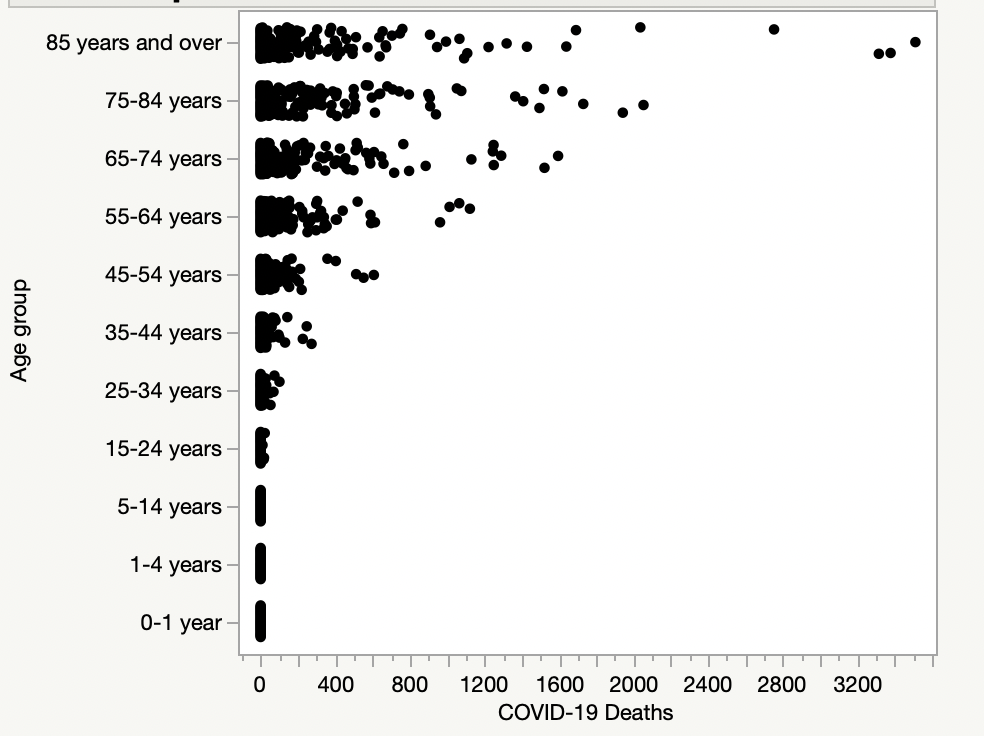
Figure 2. Age-deaths scatterplot
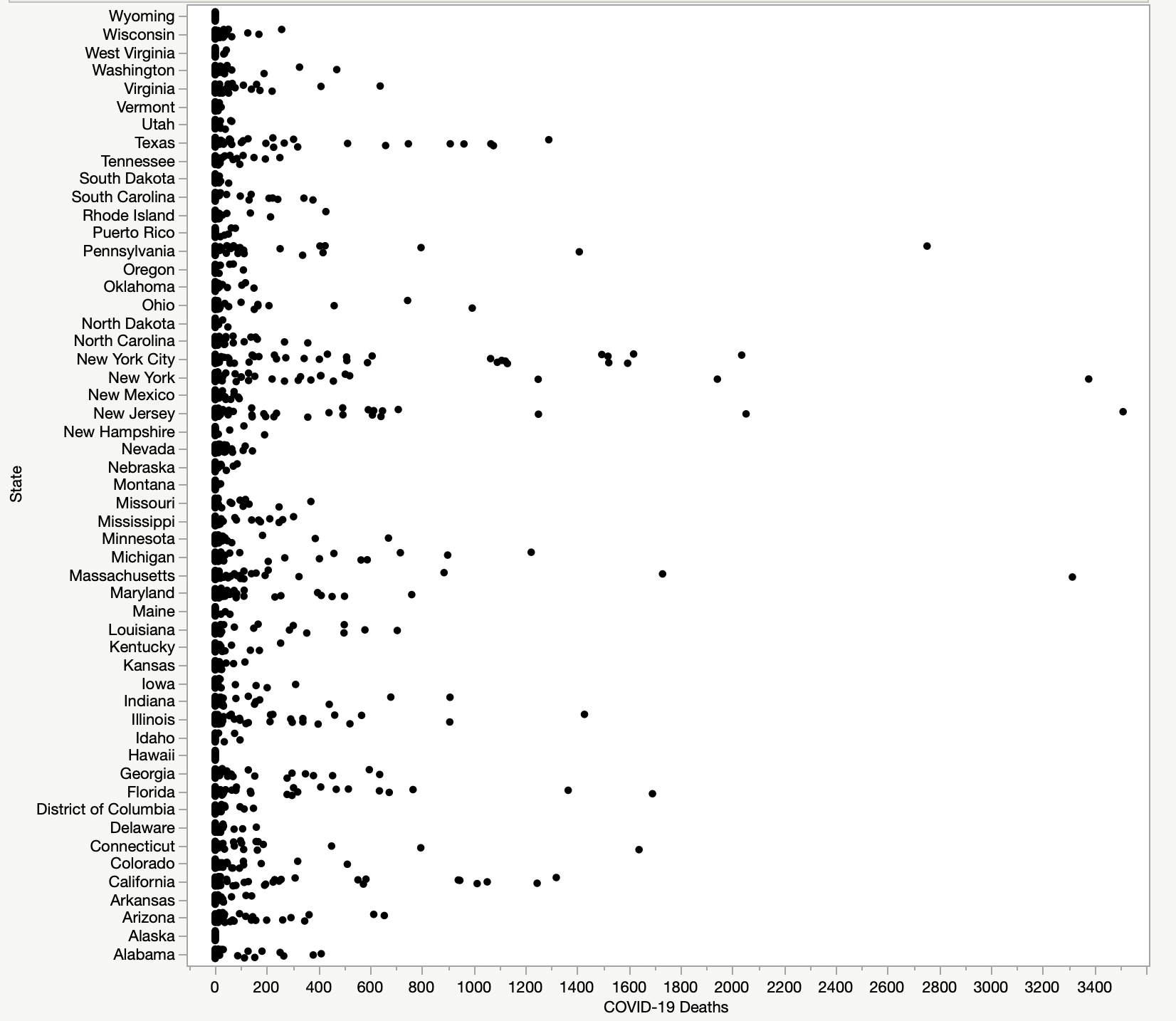
Figure 3. States-deaths scatterplot
New Jersey, New York, Michigan, Pennsylvania, Florida, California, and Texas were found to have a large variation in deaths per Figure 3. A multiple linear regression analysis showed that residence state/race-except Blacks/age were all significant with COVID-19 deaths with p-value< 0.0001.
Our second US model was found to be significant with a p-value<0.0001. Figure 4 demonstrates that both males and females experienced a similar variation in deaths. The analysis showed that age groups and residence-states were statistically significant (p-value< 0.05), while gender was not.
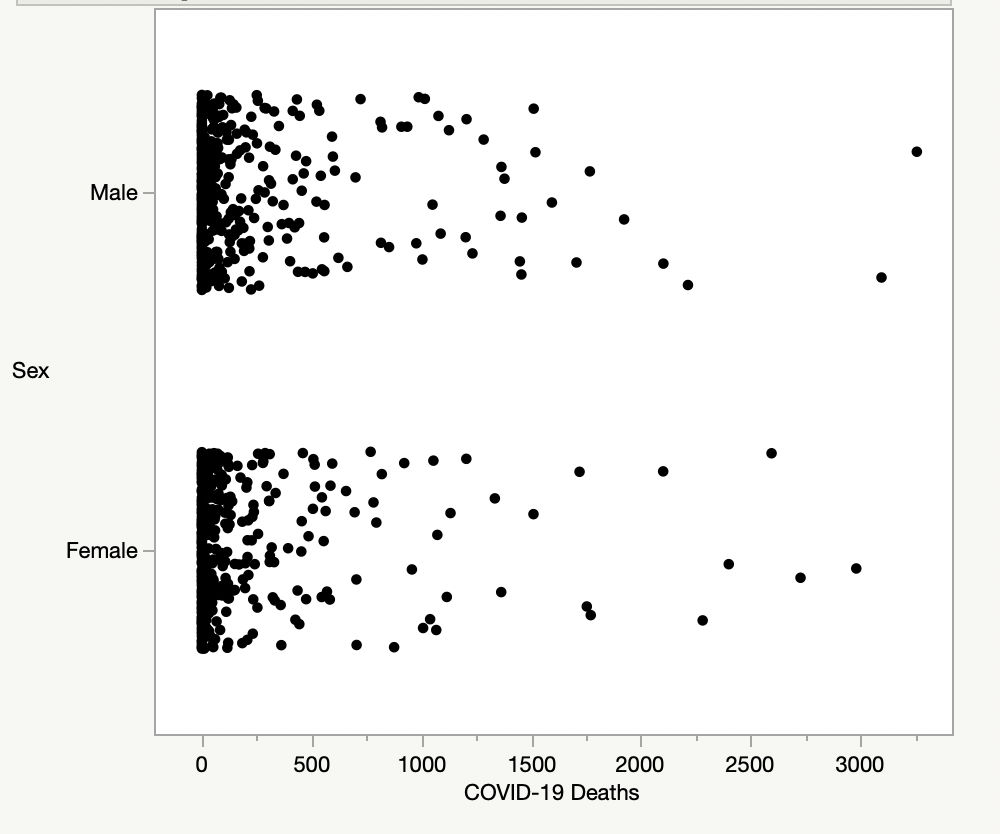
Figure 4. Gender-deaths scatterplot
2.3. India analysis
For India, Figure 5 scatterplot shows variations between state/territory and COVID-19 deaths demonstrating that Maharashtra experienced higher deaths.
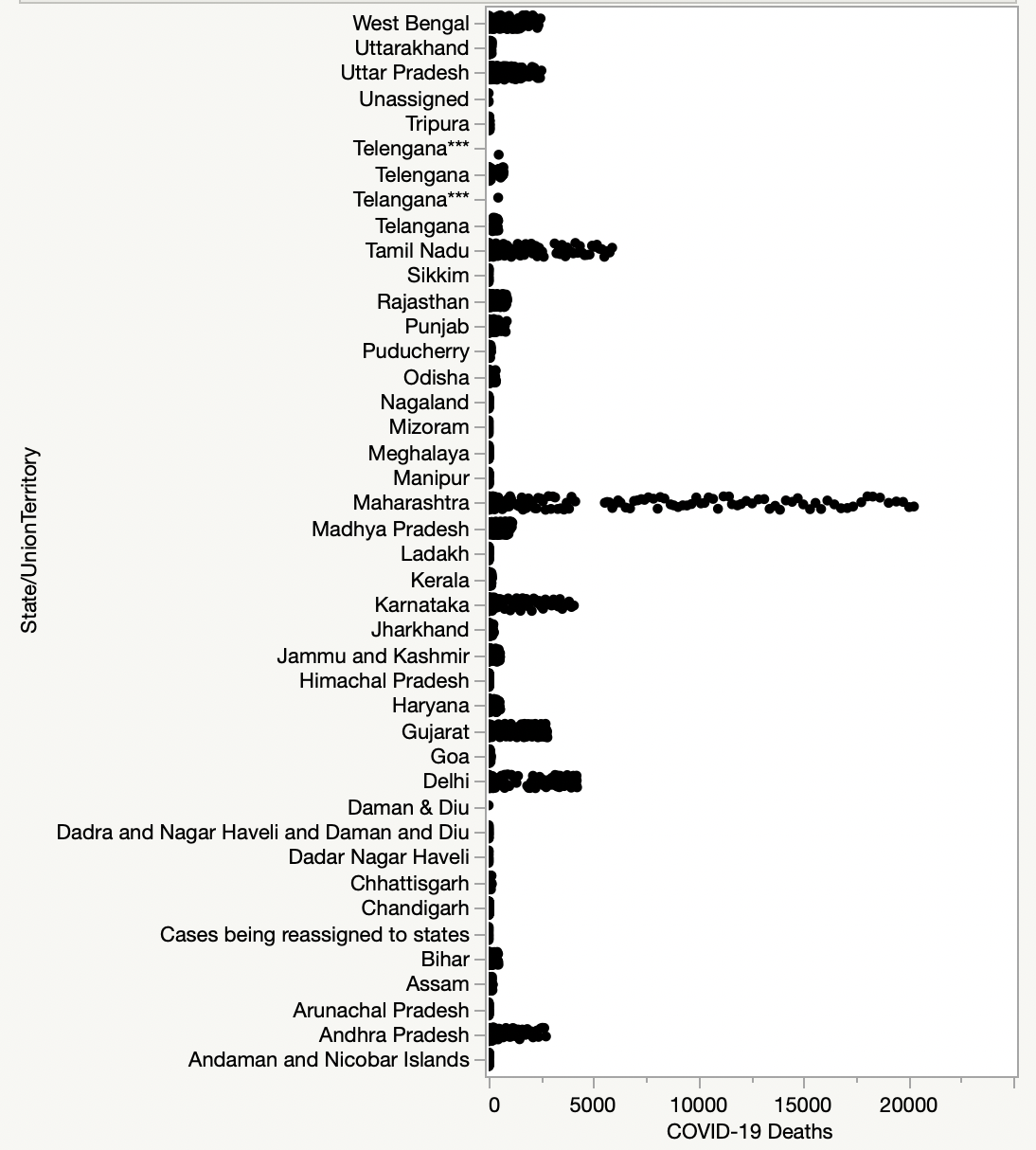
Figure 5. States-deaths scatterplot
A linear regression analysis showed that states/territories were significant with deaths with a p-value<0.0001 while Figure 6 shows both Males and Females experiencing similar variations.
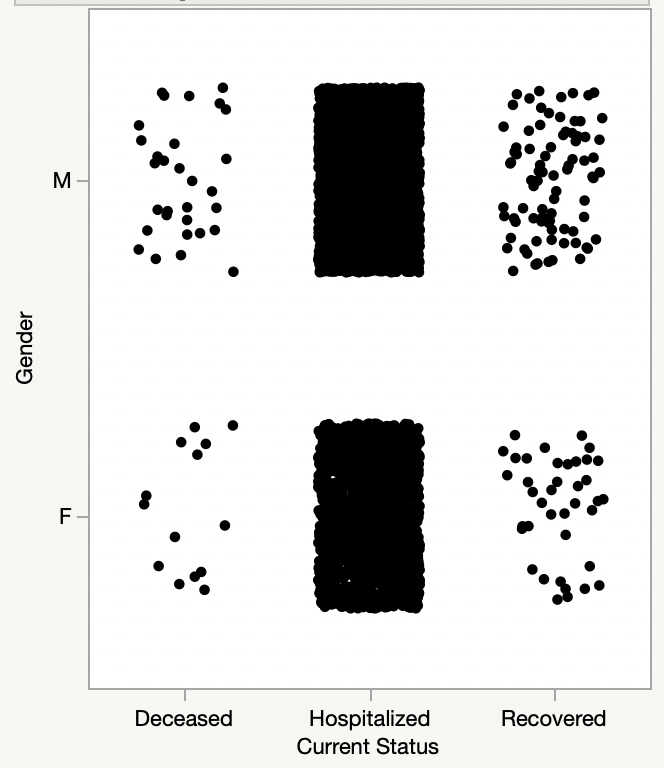
Figure 6. Gender current-status scatterplot
Figure 7 shows an increase in the number of deaths as a function of age confirming that for the age<40 your chance of death is very small.
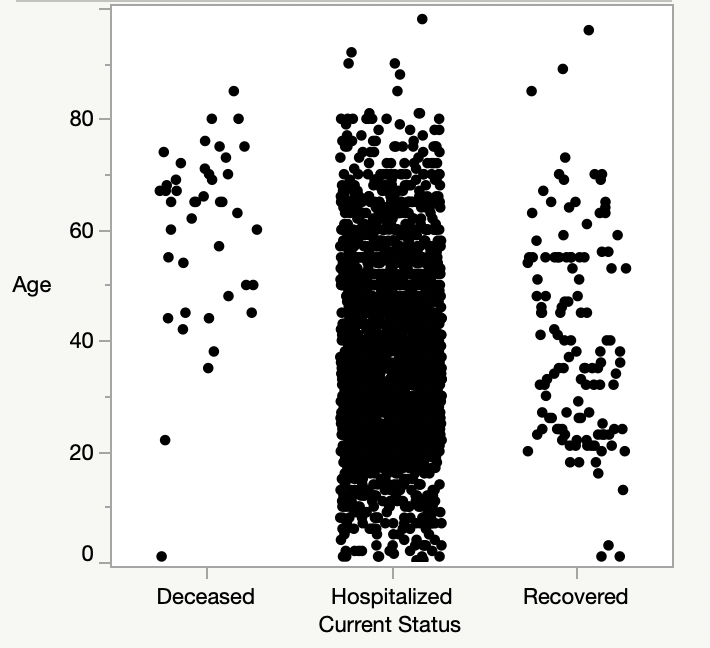
Figure 7. Age-current status scatterplot
Figure 8 shows the Receiver-Operating-Characteristics (ROC) plot. The area under the curve is the indicator of the goodness of fit. All three curves show area closer to 1 meaning a very good fit; a value=1 indicates a perfect fit.
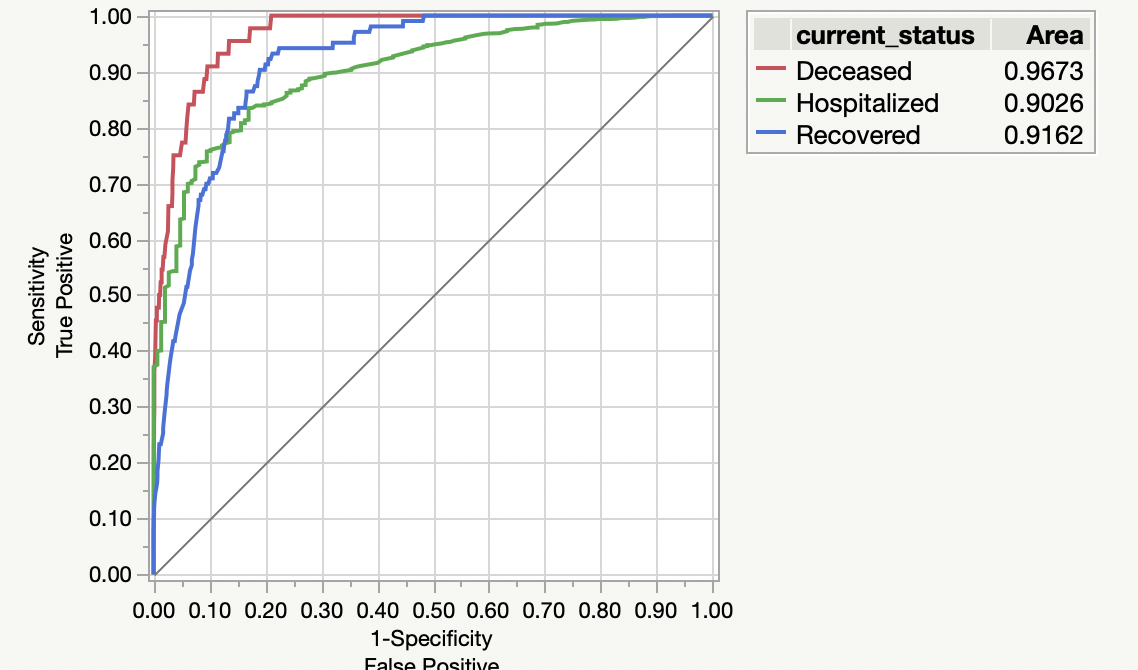
Figure 8. ROC
The second data set was run again for nominal logistics regression as shown in Figure 9. The lower curve shows the predictive probability of individual being diseased due to the virus versus the age. The rising of the lower curve shows the higher the age, the higher the predictive probability of being diseased. The upper curve shows the predictive probability of diseased or hospitalized individuals.
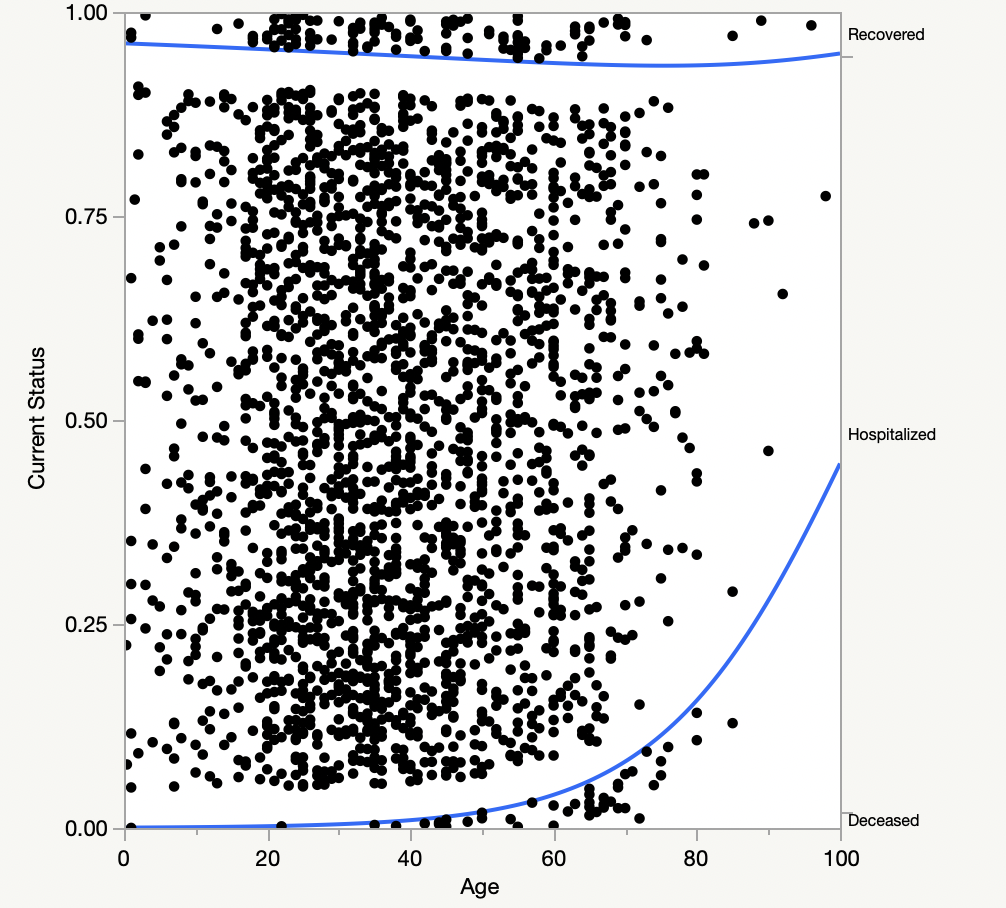
Figure 9. Logistics curve
3. USA-Social Implications
First, we propose Qualitative socio-economic Logic based Cascade Hypotheses (QLCH) related to education/occupation/and income. Second, we extend them to ‘COVID-19 deaths related to race’ hypotheses. We next look at US government’s socio-economic data of education/occupation/income/and residence place in reference to race/ethnicity to validate these hypotheses.
3.1 QLCH for a race
QLCH1: A race with lower Highschool dropouts will have higher college education.
QLCH2: A race with higher college enrollment will have higher Bachelor’s in STEM (Science/ Technology/Engineering/and Mathematics).
QLCH3: A race with higher Bachelor’s in STEM will have higher proportions of Management/professional jobs instead of Service jobs (including essential-work-hospitals/transportation/farm/grocery stores).
QLCH4: A race with a higher proportion of Management/professional jobs will earn higher median incomes.
3.2 QLCH to COVID-19
QLCH5: A race with higher median incomes will have higher percentage of private health coverage.
QLCH6: A race with higher proportions of Management/professional jobs have a better capacity to social distance by working from home.
QLCH7: A race with higher proportions of Management/professional jobs have a better capacity to social distance by living in non-crowded neighborhoods like suburbs.
QLCH8: A race with higher proportions of living in suburbs instead of cities will have better healthcare.
3.3 USA Socio-economic data
Tables 1 through 5 display socio-economic data from various U.S. Government reports [13-17].
Table 1. Graduation and jobs percentages by race in the US: 2016
| Percentage | ||||
| White | Black | Asian | Hispanic | |
| Highschool dropout rate | 5 | 6 | 2 | 9 |
| Highschool completion rate | 94 | 92 | 97 | 89 |
| Highschool dropouts who are full time job holders | 58 | 39 | 78 | 65 |
| Highschool graduates who are full time job holders | 68 | 66 | 80 | 72 |
| College enrollment rate | 42 | 36 | 58 | 39 |
| Bachelor’s awarded in STEM* | 18 | 12 | 33 | 15 |
*STEM: Science/Technology/Engineering/and Mathematics
The QLCH1 and QLCH2 apply well as shown in Table 1[13] to all four races and profoundly to Asians.
The data in Table 2 [14] shows that all races do follow QCH3.
Table 2. U.S. Bureau of labor statistics – 2019
| Occupation | M, Total employed | Percent total employed | |||||
| Female | Male | White | Black | Asian | Hispanic | ||
| Total (16 years and over) | 157.5 | 47.0 | 53.0 | 77.7 | 12.3 | 6.5 | 17.6 |
| 1) Management/professional | 64.2 | 51.8 | 48.2 | 79.0 | 9.6 | 8.7 | 10.1 |
| 2) Service: Total | 27.0 | 57.6 | 42.4 | 72.2 | 17.1 | 5.9 | 25.0 |
| 2.1) Healthcare support | 3.8 | 86.9 | 13.1 | 64.2 | 26.7 | 5.1 | 19.1 |
| 2.2) Protective service | 3.1 | 22.1 | 77.9 | 73.9 | 20.3 | 2.2 | 15.3 |
| 2.3) Food preparation and serving | 8.4 | 54.5 | 45.5 | 73.7 | 13.9 | 6.9 | 27.0 |
| 2.4) Building and grounds cleaning/maintenance | 5.7 | 42.0 | 58.0 | 77.3 | 14.9 | 2.9 | 38.2 |
| 2.5) Personal care and service | 6.0 | 76.9 | 23.1 | 69.4 | 16.1 | 10.1 | 18.2 |
| 3) Sales and office | 33.4 | 60.6 | 39.4 | 78.1 | 13.0 | 5.2 | 17.1 |
| 4) Natural resources, construction, and maintenance | 14.3 | 5.4 | 94.6 | 86.2 | 7.7 | 2.2 | 31.9 |
| 5) Production, transportation, and material | 18.6 | 23.0 | 77.0 | 74.2 | 16.9 | 5.0 | 23.0 |
For all four races QLCH5 applies well per Table 3 [15].
Table 3. Health Insurance Coverage in the United States: 2018
| Coverage | Percentage | |||
| White | Black | Asian | Hispanic | |
| Health insurance | 94.6 | 90.3 | 93.2 | 82.2 |
| Private insurance | 74.8 | 55.4 | 73.1 | 49.6 |
| Public insurance | 33.2 | 41.2 | 26.1 | 36.5 |
Table 4. Life expectancy by race: 2017
| Age | Life expectancy in years | |||
| All races | White | Black | Hispanic | |
| At birth | 78.6 | 78.5 | 74.9 | 81.8 |
| At age 55 | 27.4 | 27.3 | 25.2 | 29.8 |
Table 4 shows CDC’s life expectancy by race at birth and at 55 years [16]. Blacks had the lowest life expectancy, while Hispanics had the highest life expectancy.
Table 5 displays real median household income from the U.S. Census Bureau’s Current Population Survey [17].
Table 5. Real median household income by race in 2017 dollars
| Year | Median income | ||||
| All races | White | Black | Asian | Hispanic | |
| 2017 | $61,400 | $68,200 | $40,300 | $81,400 | $50,500 |
| 2002 | $58,000 | $64,500 | $40,300 | $72,000 | $45,000 |
| 1987 | $53,000 | $57,500 | $32,000 | $67,000 | $40,000 |
2002-2017 Annual Growth 0.38% 0.37% 0.00% 0.82% 0.77%
Table 6. Real median household income-relative to Asians
| Year | Median income | ||||
| All races | White | Black | Asian | Hispanic | |
| 2017 | 0.75 | 0.84 | 0.50 | 1.00 | 0.62 |
| 2002 | 0.81 | 0.90 | 0.56 | 1.00 | 0.63 |
| 1987 | 0.79 | 0.86 | 0.48 | 1.00 | 0.60 |
Average 0.78 0.87 0.51 1.00 0.62
From Table 5, we converted real median household income in terms of Asians as shown in Table 6. Over a 30 year period, Blacks made 51 cents on a dollar, Hispanics made 62 cents on a dollar, and Whites made 87 cents on a dollar versus Asians. Thus QLCH4 applies well to all four races.
3.4 Socio-economic implications of race and living location to COVID-19
Applying QLCH6, Asians/Whites with higher proportions of Management/professional jobs instead of Service jobs do have better capacity to social distance by working from home while the opposite is true for Blacks/Hispanics.
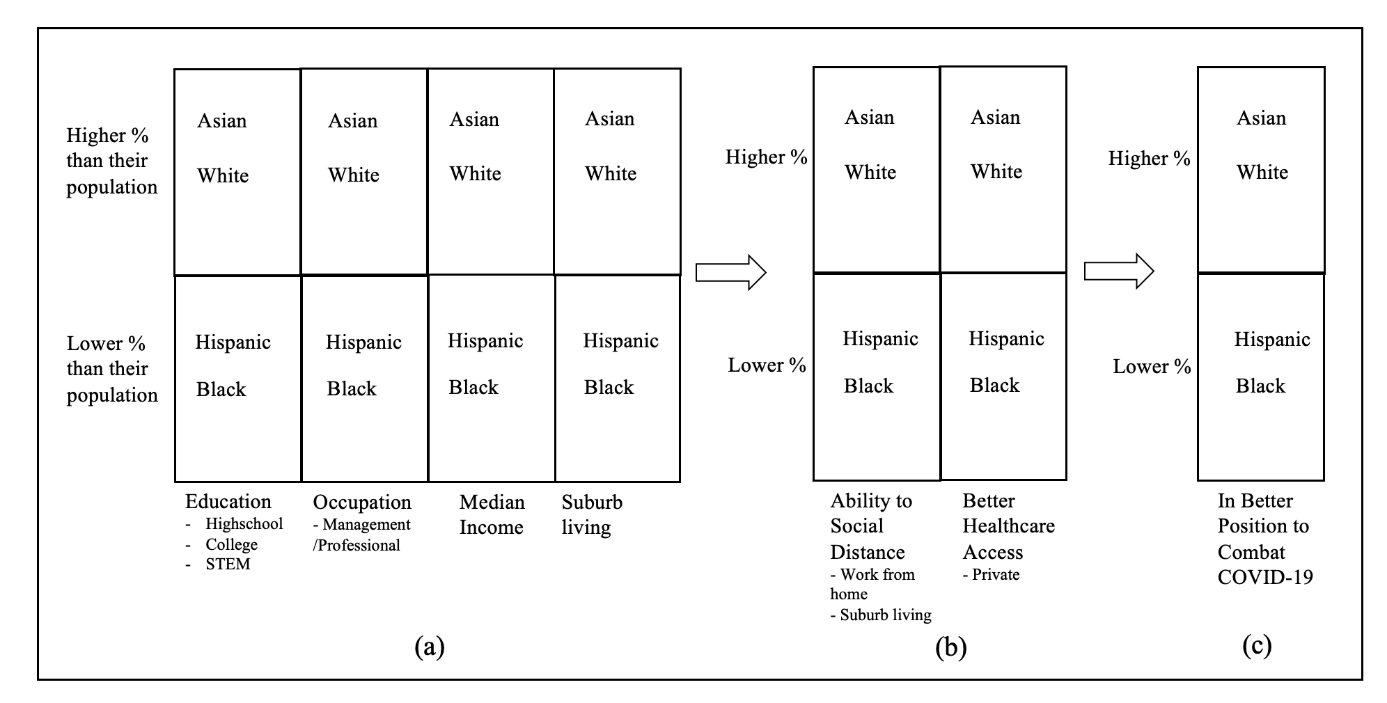
Figure 10. Race/ethnicity based socio-economic implications for COVID-19
Considering QLCH7, Asians/Whites with higher proportions of Management/professional jobs do have better capacity to social distance by living in non-crowded neighborhoods like suburbs versus Blacks/Hispanics.
Utilizing QLCH8, Asians/Whites with higher proportions living in non-crowded neighborhoods, such as more suburban areas, have better healthcare access versus Blacks/Hispanics.
Figure 10 summarizes race/ethnicity based socio-economic implications for COVID-19. In Figure 10(a) Asians/Whites versus Hispanics/Blacks have higher percentages in education including STEM leading to higher percentages in Management/professional jobs instead of Service/essential jobs, leading to higher median incomes. Higher median incomes give them the choice of living in more suburban areas. This allows higher percentage of Asians/Whites, versus Hispanics/Blacks, the ability to social distance by living in suburbs as well as working from home -see Figure 10(b). This leads to Asians/Whites being better positioned to combat COVID-19 -see Figure 10(c).
3.5 Comparison of regression analyses with socio-economic analysis
Our two regression analyses showed that where you live/state and race are statistically significant with COVID-19 deaths for the US. These analyses are in concert with the QLCH analyses based conclusions for both race/ethnicity and residence-states supported by Tables 1 through 5.
4. Understanding Indian socio-economic conditions
Table 7 depicts India’s top populated states with ranking based on urban population [12a].
Table 7. India’s top 10 populated states
| State | Urban Rank | Urban Population | Total Population |
| Maharashtra | 1 | 50.8M | 112.4M |
| Uttar Pradesh | 2 | 44.5M | 199.8M |
| Tamil Nadu | 3 | 34.9M | 72.1M |
| West Bengal | 4 | 29.1M | 91.3M |
| Gujarat | 5 | 25.7M | 60.4M |
| Karnataka | 6 | 23.6M | 61.1M |
| Madhya Pradesh | 7 | 20.1M | 72.6M |
| Rajasthan | 8 | 17.0M | 68.5M |
| Andhra Pradesh | 9 | 14.6M | 49.6M |
| Bihar | 10 | 11.8M | 104.1M |
We created Table 8 with the COVID-19 death rankings derived from Figure 5 and added GDP rankings [13a]. These rankings for the residence-states match well with urban population and GDP rankings. GDP creation requires people to interact with others as close proximity realized in higher urban density setting would exacerbate the social distancing issues faced by the population.
Table 8. India’s top 10 COVID 19 death states
| State | Urban Rank | GDP Rank | COVID-19 Death Rank |
| Maharashtra | 1 | 1 | 1 |
| Uttar Pradesh | 2 | 5 | 6 |
| Tamil Nadu | 3 | 2 | 2 |
| West Bengal | 4 | 6 | 7 |
| Gujarat | 5 | 3 | 4 |
| Karnataka | 6 | 4 | 3 |
| Madhya Pradesh | 7 | 11 | 8 |
| Rajasthan | 8 | 8 | 9 |
| Andhra Pradesh | 9 | 7 | 5 |
| Bihar | 10 | 15 | 10 |
5. Conclusions
For the US, by July 2021, COVID-19 deaths have already exceeded 620,000. Demographic factors of age groups/race/residence state were found to be statistically significant in our analyses. The virus does affect both genders equally and an individual’s age is a critical variable deciding life/death, for age of 55 and above. Race/ethnicity seems to play an important role also, as Blacks and Hispanic death proportions are higher than their respective population proportions. Bigger population states with high minority populations have seen higher deaths. Thus, inequality in socio-economic conditions is an important determinant affecting health conditions of an individual and, more importantly, his/her ability to social distance at work or at home. Socio-economic analysis for the US population shows that QLCH of education/occupation/and income affects race/ethnicity differently. For a given race/ethnicity, education drives occupation then income, living location, and in turn his/her access to healthcare. Considering the US socio-economic data in the QLCH framework, we conclude that different races are poised for differing effects of COVID-19. In particular, Asians/Whites are in a better position to combat COVID-19 compared to Hispanics/Blacks.
India with 0.73% death rate witnessed about 10M total deaths in 2020. The COVID-19 deaths by August 2021 has exceeded 420K. We observed that the residence-states/territories are a significant factor. The top 10 states experiencing deaths are found to be in top 10 urban population ranked states coupled with top 15 GDP creation. Case in point is Maharashtra with urban population rank 1st and GDP rank 1st had highest COVID-19 caused deaths in the country. The state of Tamil Nadu with urban population rank of 3rd and GDP rank of 2nd had the second highest deaths. Forced avoidance of social distancing in larger urban and high GDP creating states may be the driver in getting higher COVID-19 infections. Factors of age, and residence-states were found statistically significant using logistical regression, however, gender was found to be not. The data showed that virus does not spare any gender over other. The age is a critical variable that decides death over life and is pronounced especially for age>40. Focusing solely on 420K deaths due to COVID-19 through August 2021 misses the remaining bigger picture of 10M annual deaths caused by many other issues in India.
6. References
1. Heron M. National Vital Statistics Reports Volume 68, Number 6, June 24, 2019, Deaths: Leading Causes for 2017. https://www.cdc.gov/nchs/data/nvsr/nvsr68/nvsr68_06-508.pdf
2. Our World In Data https://ourworldindata.org/country/india, 28 August 2020
And
https://ourworldindata.org/coronavirus/country/india?country=~IND, 28 August 2020
3. Pareek M, Bangash MN, Pareek N, et al. Ethnicity and COVID-19: an urgent public health research priority. The Lancet Volume 395, Issue 10234, P1421-1422, May 02, 2020. https://pubmed.ncbi.nlm.nih.gov/32330427/
4. Rentsch CT, Kidwai-Khan F, Tate JP, et al. Covid-19 by Race and Ethnicity: A National Cohort Study of 6 Million United States Veterans. Preprint. medRxiv. 2020;2020.05.12.20099135. Published 2020 May 18. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7273292/
5. Vahidy FS, Nicolas JC, Meeks JR et al. Racial and Ethnic Disparities in SARS-CoV-2 Pandemic: Analysis of a COVID-19 Observational Registry for a Diverse U.S. Metropolitan Population. medRxiv 2020.04.24.20073148; https://www.medrxiv.org/content/10.1101/2020.04.24.20073148v2
6. Millett GA, Jones AT, Benkeser D, et al. Assessing differential impacts of COVID-19 on black communities. Annals of Epidemiology, Volume 47, July 2020, Pages 37-44. https://www.sciencedirect.com/science/article/pii/S1047279720301769
7. Acharya, R., Porwal, A. “A vulnerability index for the management of and response to the COVID-19 epidemic in India: an ecological study.” The Lancet Issue 9, Volume 8, E1142-E1151, September 01, 2020. Web.
8. Kamath S, Kamath R, et al. “COVID-19 pandemic in India: challenges and silver linings.”
Postgraduate Medical Journal 2020;96:422-423.
9. Centers for Disease Control and Prevention, Deaths involving coronavirus disease 2019 (COVID-19) by race and Hispanic origin group and age, by state. Accessed 20 August 2020. https://data.cdc.gov/NCHS/Deaths-involving-coronavirus-disease-2019-COVID-19/ks3g-spdg.
10. Centers for Disease Control and Prevention, Provisional COVID-19 Death Counts by Sex, Age, and State. Accessed 20 August 2020. https://data.cdc.gov/NCHS/Provisional-COVID-19-Death-Counts-by-Sex-Age-and-S/9bhg-hcku
11. “Kaggle.” https://www.kaggle.com/sudalairajkumar/covid19-in-india?select=covid_19_india.csv, 28 August 2020
12. “Kaggle.” https://www.kaggle.com/sudalairajkumar/covid19-in-india?select=IndividualDetails.csv, 28 August 2020
13. de Brey C, Musu L, McFarland J, National Center for Education Statistics, U.S. Department of Education, NCES 2019-038. Status and Trends in the Education of Racial and Ethnic Groups 2018. Accessed 20 August 2020. https://nces.ed.gov/pubs2019/2019038.pdf
14. U.S. Bureau of Labor Statistics, Labor Force Statistics from the Current Population Survey HOUSEHOLD DATA
ANNUAL AVERAGES 11. Employed persons by detailed occupation, sex, race, and Hispanic or Latino ethnicity. Accessed 20 August 2020. https://www.bls.gov/cps/cpsaat11.pdf
15. Berchick ER, Barnett JC, Upton RD. Health Insurance Coverage in the United States: 2018. Issued November 2019 P60-267(RV). Accessed 20 August 2020. https://www.census.gov/content/dam/Census/library/publications/2019/demo/p60-267.pdf
16. Centers for Disease Control and Prevention, National Vital Statistics Reports Volume 68, Number 9 June 24, 2019 Deaths: Final Data for 2017. Accessed 20 August 2020. https://www.cdc.gov/nchs/data/nvsr/nvsr68/nvsr68_09-508.pdf
17. U.S. Census Bureau, Current Population Survey, 1968 to 2018 Annual Social and Economic Supplements. Real Median Household Income by Race and Hispanic Origin: 1967 to 2017. Accessed 20 August 2020. https://www.census.gov/content/dam/Census/library/visualizations/2018/demo/p60-263/figure1.pdf

