Abstract
This bibliographic review evaluates Artificial Intelligence (AI) theory’s applications in the field of Family Medicine. Globally billions of people suffer from multiple health related issues throughout their lives including diseases of the heart, lungs, kidney, diabetes, and many forms of cancer. Diagnosis, remedy, and prevention of these disorders are multifaceted, and machine/computer based investigative tools for doctors are immediately needed to augment their decision-making. This study includes various applications of AI/machine learning (AI/ML) procedures in family medicine and its various sub-specialties. AI/ML-centered medicine offers better solutions over standard family medicine covering birth throughend of life care. These include treatments for adolescents, geriatrics, disorders of pain and sleep, and sports injuries. However, several implementation hurdles for AI in clinical family medicine persist. Keywords: AI and machine learning in family medicine, AI and machine learning in geriatrics, AI and machine learning in disorders of pain and sleep, AI and machine learning in sports injuries.
Introduction
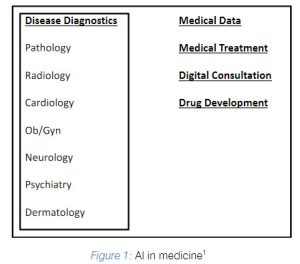
he main objective of this paper is to appraiseapplications of Artificial Intelligence (AI) andMachine Learning (ML) in the field of familymedicine.Since1990stherehas been majoradvancements in the use of AI to images based fields of medicine(e.g. radiology, pathology, and ophthalmology,..).
In the field of Family Medicine, AI has applications in disease diagnostics and prevention in numerous subspecialties (Figure 2).
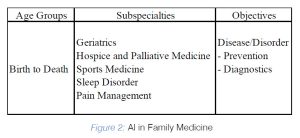
In this article, first we reviewed AI-based family medicine research in various clinical situations that are included in Figure 2. Secondly, different ethical and
social issues of Artificial Intelligence, for use in various family medicine presentations, are discussed.
Artificial Intelligence or AI
Artificial Intelligence or AI is an intelligence that is artificial and not natural. AI is established on several statistical ideologies in which an observation is ‘learned’by a computer or a machine. The understanding of the observation bya machine gets smarter as more learning by the machine takes place. After an appropriate extent of this training, Artificial Intelligence, as a human being, becomes suitable for crafting decisions. In this section the main AI terms and ML-based algorithms are described.
a) AI Fundamentals In this section, essential AI terms are concisely reviewed.2
Machine learning (ML) methodology brings statistical modeling and a machine (computer) together in order to learn from available information. Machine Learning is categorized into ‘supervised’ and ‘unsupervised’ learning.
i. Supervised learning technique constructs a forecast model based on known output and input data values. The model is then applied to forecast new
output for a specified new input information. Supervised learning is applicable for both i) a ‘classification’ model for output classifications (e.g., a patient has cancer or patient is cancer- free based on an MRI image) and ii) a ‘regression’ model for a continuous output variable (e.g., patient’s cholesterol level).
ii. Unsupervised learning technique is applicable when there is no output prediction variable present and input data is not labeled. This approach groups
data together, to comprehend the intrinsic structure of the data, based on their resemblances (e.g., clustering patterns in a sample of patients with an
illness that could lead to new drug therapy).
iii. Semi-supervised learning is a fusion of ‘Supervised’ and ‘Unsupervised’ learning methodologies. Artificial Neural Networks or ANNs accomplishes an
output forecast that results from several independent partsof calculations and weightings. ANN, analogous to a network of neuron inside a brain, has a set of artificially layered/connected neurons to transfer information across the network.
b) ML Algorithms Supervised Machine Learning contains the splitting of the accessible information into both ‘training’ and ‘examination’ sets for uthentication of the algorithm. In this type of machine learning, the following algorithms are broadly employed:
a) Regression: For machine learning, both ‘linear regression’ (use of least squares regression line between ‘the cause’ or independent variables and ‘the effect’ or dependent variables), and ‘logistic regression’ (applied for binaryconclusions of ‘yes or no,’ or ‘no illness or illness’ with classifications of
either categorical or continuous) techniques are frequently used and are built on data types.
b) Decision Tree (DT): The decision tree-based algorithm includes a set of procedures that describe the route from‘the root’ to ‘the leaves’.
c) Naive Bayes: Naïve Bayes algorithm hypothesizes that the characters under evaluation are independent of eachother.
d) Support Vector Machine (SVM): The SVM-based machine learning algorithm discovers a nonlinear association and classifies data by relating a
hyperplane that best differentiates the presence of two collections.
e) k-Nearest Neighbor (k-NN): This ML algorithm is used for data classification of nonparametric grouping. The ‘k’, is the square root of the number of
occurrences and its isolation from a pre-selected point.
f) Random Forest (RF): Random Forest based ML algorithm, prevents ‘overfitting’ and is an effective tool for a precise appraisal of classifiers. However, these algorithms are less capable than the SVM and k-NN based methods.
g) Convolutional Neural Networks (CNNs): ‘Convolution’ is a system of a mathematical function on two functions that produces a third function.
CNNs learn by several duplications of both ‘analyzing’ and ‘weighting’ the patterns it identifies in the pictures.
AI in Family Medicine
Family medicine professionals’ work includes the diagnosis or identification of a disease followed by its prognosis (or a prediction of the course of the
disease including the treatment and outcomes), and if needed, referring patients to appropriate specialists, providing care to patients with empathy, and
documenting the data. Globally, over the pastfew years, AI is being evaluated for its application in family medicine.
In 2018, Blease et al. conducted a cross sectional survey of 1,474 General Practitioners (GPs) in the United Kingdomabout the computerization and the
future of primary care. About half (720) of the GPs replied to this survey. Majorityout of them responded that AI will unlikely be able to replace doctors for diagnosing patients (68%), devising custom- made treatment strategies (61%), referring patients to specialists (61%), and providing compassionate care (94%).
However, about half of the family physicians (53%), who answered the survey, believed that technology can completely replace doctors for the purposes of prognostics of a disease. Also, a significant majority of the respondents(80%) believed that AI will be able to replace doctors for the purposes of medical
documentation.3
Summerton et al., in 2019, observed that clinical information obtained from patients in family practice is ill-defined. This is where AI’s language processing
techniques can provide the tools to analyze unstructured data from patients’ records. AI, per the authors, being a focused technology has on surface
inconsistency with the comprehensive nature of family medicine. The authors believe that AI can assist in the projecting value of symptoms which is explicit
knowledge. However, according to them, tacit knowledge such as how to obtain a patient’s confidence is where AI may fall short.4
In 2021, Baser et al. evaluated the artificial intelligence related anxiety of family physicians in Turkey. The sample size for the study included 402 family physicians. Even though most doctors have no formal training on AI based applications, their anxiety levels were low. The authors therefore concluded that a
structured AI based training program for applications in family practice can contribute as a decision support system and can enhance patient safety.5
Darcel et al. in 2023 studied the obstacles that Canadian patients (n=22), health providers (n=21), and health leaders (n=5) recognize with respect to applying AI in primary care based medicine. Major obstacles in implementing AI included (a) readiness of system and data, (b) the possibility for inequity and bias, and (c) the rules of AI. For each of these categories respondents were concerned about trust in the AI technology itself or in the health provider applyingit.6
In 2020, Liaw et al.’s study concluded that AI based tools are not disposed for realization yet. There are significant consequences for confidentiality, misuse,
and overtreatment with applying AI. In order for AI to be widely used in family medicine, the family practice physicians need to partake in appropriate plan, strategy, research, and delivery approaches. The authors also stressed that personal connections are more important than computer based tools.7
a) AI in Diabetes Detection in Family Medicine Globally diabetes affects hundreds of millions of people. In the US the count is around 40M, with approximately 1.4M people diagnosed with the disease annually, and causes more than 100,000 deaths per year. The disease costs annually around $340B which includes $240B in medical costs and $100B in loss in productivity. An early detection and timely medical treatment of various types of diabetes (type 1, type 2, and gestational) is therefore important.
Wei et al.’s work in 2010 utilized electronic clinical notes from Mayo Clinic and combined ‘Natural Language Processing’ (NLP), ‘ML,’ and ‘Ontology’ to
automatically associate it to patients. Their AI model attained an F- score larger than 0.95 for both type 2 diabetes mellitus and control groups when utilizing all identified concept units (semantic type-Disease or Syndrome) as characters.8 Shankaracharya et al.’s research in 2012, from India, used the health reports of 1,415 hospitalized patients that were classified as either ‘diabetic’ or ‘nondiabetic’.
A new ML algorithm, named “mixture of expert,” was used by the authors for training based on 1,104 patients’ diabetic state, while 311 patients’ data
was kept for authentication of the algorithm. The model produced excellent sensitivity (99.5%), specificity (99.07%), and total classification accuracy (99.36%) for classifying ‘pre-diabetic,’ ‘diabetic,’ and ‘non-diabetic’ individuals.9
b) AI in Heart Disease Detection in family medicine Annually, heart disease causes about 700K deaths in the US. To reduce these deaths, an early detection and treatment of the disease is therefore critical. In 2020, Choi et al. evaluated ‘AI-Clinical Decision Support System’ (AI-CDSS) for assisting doctors in diagnosing of heart failure which is a difficult task. The AI-CDSS model included a combination of ‘expert-driven’ and ‘ML- driven’ methods to advance the
knowledge base for the diagnosis of heart failure. The model utilized a retrospective unit of 1,198 patients (training: n=600 and testing: n=598) with and without heart failure for the AI-CDSS model development and evaluation of its performance. The concordance rate, which is the probability that a pair of individuals will both have a certain characteristic (given that one of the pair has the characteristic), between ‘AI-CDSS model’ and ‘heart specialists’ was 98%, while that between ‘heart specialists’ and ‘non-heart specialists’ was 76%. Thus, AI-CDSS may be helpful to the ‘non-heart specialists’, such as family physicians for the heart failure diagnosis when the heart specialists are not available.10
c) AI in Cancer Detection in Family Medicine In the US, cancer causes more than 600K deaths annually. To reduce these deaths, an early detection and treatment of the disease is therefore important. Hamilton et al. in 2013 noticed that diagnostic delay for cancer appeared to have contributed to about
5,000 to 10,000 additional deaths annually in the UK. Risk assessment tools (RATs) for selecting patient for evaluation of lung and colorectal cancer diagnoses were established to help GPs. The study included 614 GPs who were provided RATs for 2,593 patients with either respiratory (n=1,160) or bowel (n=1,433) related symptoms. In comparison with the preceding six months, 292 additional X-rays produced 47 more diagnoses for lung cancer. Similarly an additional 270 colonoscopies yielded identification of 10 more cancers. Thus the application of RATs based AI produced enhanced diagnostic activity in primary care for additional diagnoses of cancer.11 In 2019, in England an AI based novel diagnostic tool ‘C the Signs’ that assists in cancer detection was given to 1,000+ GP practices. The AI tool supported in GP consultation for a) advising on what to investigate, and b) referrals the patient may require. In
east England, a pilot run of ‘C the Signs’ demonstrated an amplified cancer detection rateof 6.4% versus 0.21% in non-pilot practices.12
d) AI in Depression in Family Medicine Feeling unhappy, having low interest in normal activities, and further comparable symptoms for at least
two weeks all can be the signs and symptoms of depression.
Kurian et al.’s work during 2005 and 2006 focused on a clinical trial of primary care facilities in Texas to assess a computerized decision support
system (CDSS) which included 55 patients with major depressive disorder (MDD). The physicians utilized CDSS to treat 32 patients while the remainder 23
patients received usual care. The CDSS employed patients saw a appreciably superior symptom decrease, based on the 17-item Hamilton Depression Rating Scale or HDRS(17), versus patients that received the usual care with a p-value < 0.001.13
In 2021, Tanguay-Sela et al.’s research assessed Aifred, a CDSS which utilizes AI to help doctors in choosing treatments for patients with MDD, established on patient characteristics. Twenty physicians (residents in either psychiatry or family medicine) in this study, each had three clinical communications with patients depicting mild, moderate, and severe incidents of MDD. These physicians had availability of the CDSS for their treatment choices. Overall 60% of them professed that the CDSS is a valuable tool in their process of treatment-finalization, with family medicine doctors recognizing the highest utility. In addition, they found the AI tool to be suitable in reviewing treatment choices with patients.14
e) AI in Attention Deficit Hyperactivity Disorder (ADHD) A person with attention deficit hyperactivity disorder (ADHD) illness has variations in the
development of brain and brain activity from a typical brain, which disrupts attention, and the ability to sit motionless. It is important to diagnose patients with signs of ADHD as soon as possible to provide them with efficient treatment.
During 2019-2020, Loskutova et al.’s research analyzed a web-based ‘American Academy of Family Physician AdultADHD Toolkit’ comprised of tools to help
in the identification, management, and healing of adults with symptoms of ADHD. The study included evaluation of 97 primary care and behavioral health care specialists’ usage of the Toolkitfor the duration of 17 weeks. Various statistical analyses showed that the Toolkit enhanced health care professional’s knowledge versus baseline in areas for treatment effects, outcomes, existing ADHD resources with p-value < 0.05 for each. Eighty seven percent of articipants acknowledged that the Toolkit tackled most of their needs involved in identification, management, and treatment of ADHD for adults.15
f) AI in Mood Disorders in Family Medicine Type of primary care patients troubles of mood include a) major and minor depression, b) anxiety disorders, c) dysthymia, and d) bipolar spectrum disorders. These mood disorders result in increased morbidity and deaths. Their early detection and treatment is therefore important.
Nemesure et al.’s work in 2021 focused on utilizing AI to assist primary care professionals in early detection of GAD (Generalized Anxiety Disorder) and
MDD (Major Depressive Disorder). The authors applied a new ML pipeline approach which included deep learning to ‘re-analyze’ Electronic health records EHRs) based information from an observational study of 4,184 undergraduate students undertaking a health screening including a psychiatric (GAD and MDD) evaluation. The model was trained, excluding psychiatric data, with 59 ‘biomedical’ and ‘demographic’ characters from the health appraisal, and a set of engineered characters were used for model training. This trained AI model applied to test data yielded 0.73 Area Under Curve (AUC) value, 0.66 sensitivity, and 0.7 specificity for GAD (AUC of 0.67, sensitivity of 0.55, and specificity of 0.7 for MDD).16
AI in Specialties of Family Medicine
a) AI in Geriatrics
Geriatrics, the practice of care for older adults, is an important subspecialty of family medicine which focuses on. the aging process. Aging in blood and
nervous systems can accelerate a person’s probability to experience medical complications. Improving the quality of life in elderly population is therefore important. In 2021 Petrauskas et al.’s research acknowledged that the assessment of a geriatric patient is a time consuming procedure as it comprises of an
assortment of questionnaires with some times biased and erroneous patient answers. The authors considered the ‘explainable artificial intelligence’ (XAI) centered CDSS to evaluate diet-associated elements and to define the possibility of patient’s health threats linked with syndromes of a) malnutrition, b) dehydration, c) eating disorders in dementia, and d) oropharyngeal dysphagia. 83 geriatric patients from Lithuania, with diverse nutritional related health circumstances, were analyzed for the four syndromes based on CDSS, and they were compared with the judgements of the doctors attained using standard evaluation approaches. The proposed CDSS proficiently diagnosed diet associated geriatric syndromes with great accuracy of a) malnutrition: 88%, b) dehydration: 87%, c) eating disorders in dementia: 90%, and d) oropharyngeal dysphagia: 88%.17 Vaiyapuri et al.’s work, in 2021, focused on the monitoring of elderly living in smart homes for accidents such as falls. The authors devised an ‘Internet of Things’ (IoT) supported fall recognition model utilizing ‘optimal deep convolutional neural network’ (ODCNN) for smart homes where IoT devices can be used to detect and then capture falls. The falls typically can result in death due to subsequent complications. The model’s classifier distinguished between ‘fall’ and ‘non-fall’ incidents. If a ‘fall’ incident is detected, then the smartphone directs an alert to the closest hospital. The model resulted in an accuracy over 99% for both the numerous cameras fall and the UR University of Rzeszow) fall recognition data.18
b) AI in Hospice and Palliative Medicine Hospice care is ‘comfort upkeep’ deprived of healing intent, while palliative comfort care is comfort
care that can have curative intent. A family physician with specialty in hospice and palliative medicine delivers care to mitigate the distress felt by patients with ‘lifelimiting’ ailments.
In 2018, Avati et al. explored challenges posed in enhancing access to palliative care as physicians over-appraise patient prospects and there is a lack of supporting staff. The authors using ML and patients’ EHR data trained Deep Neural Network in order to forecast death of patients during the succeeding 3 to 12 months. This forecast was updated on a daily basis based on the AI model and was utilized as a decision maker for categorizing patients who could benefit from the palliative care, as the care resource availability is limited. The authors demonstrated AI’s application in palliative medicine.19
Wang et al., in 2019, developed a deep learning algorithm using longitudinal EHRs in order to forecast death risk as a proxy sign for classifying patients with dementia; this is a group who could benefit from palliative care.
This retrospective cohort study included sixmonth, twelve-month, and 24-month death forecast models which utilized patient demographic information and themes created from clinical notes from a health care delivery system in Boston, Massachusetts. The study included 26,921 patients (60.4% women, mean age, 74.6 years). The models were trained using data from 24,229 patients with a mean age of 74.8 years (60.4% women.) The remaining 2,692 patients’ data with the mean age of 75 years (60.6% women) was used for evaluation. The six-month model achieved AUC of 0.978, the 12-month model with 0.956, and the 24- month with 0.943. Their algorithm based on a) patient demographic information and b) clinical notes demonstrated encouraging results in forecasting death among patients with dementia in distinctive time periods.20
c) AI in Sports Medicine
A family physicians with expertise in sports medicine focuses in identifying and remedying injuries associated due to sports and exercise. This specialist also helps people with ailments that may have consequences on their well- being and physical performance.
In 2021, Rigamonti et al.’s research focused on fictitious sports injuries analysis using an AI algorithm. The five cases of acute and subacute sport-related injuries were crafted: a) concussion, b) ankle sprain, c) muscle pain, d) chronic knee instability, and d) tennis elbow. The indications of these occasions were submitted into a ‘chatbot- guided’ app and its results were associated to the pre-defined injuries. The app asked between 25 and 36 questions, requesting photos to explain the issue faced per patient for each of these cases. The cases of a) a mild concussion, b) an ankle sprain, c) a muscle pain in the thigh, and e) the condition of the chronic epicondylitis were all correctly diagnosed individually. However, for a chronic ACL instability the algorithm did not conclude the chronic characteristic of the pathology but provided a recommendation to see a doctor for further evaluation. The model thus provided an excellent tool, which either diagnoses correctly or provides correct referral to see a medical specialist.21
Novatchkov et al.’s, in 2013, evaluated the potential of AI in weight training based on 15 participants performing 3-5 sets (10-12 repetitions) on a leg press machine. The authors utilized pattern recognition procedures for the assessment of exercises performed on training machines. The machines were incorporated with sensors to measure both force and displacement, which were then used to calculate velocity and time periods. These factors as an input to ML methodologies resulted in an automatic evaluation of the workout procedure producing individuals with suitable feedback. The authors’ AI model yielded good performance in automating performance evaluation on weight training equipment and giving prompt advice to sportsman/sportswoman. 22
In 2019, Bloomfield et al.’s study focused on assessing patients going through ‘total knee arthroplasty’ with data acquired from wearable sensors. The authors utilized ML approach to analyze the data to provide and categorize patients into pertinent groups. 68 patients finished instrumented ‘timed-up-and-go’ examinations pre-operation and also at after two, six, and twelve week post-operation. Wearable sensors based system isolated 55 items for evaluation and an AI algorithm divided patients into differing categories centered on the derived characters. The 68patients were split into two groups of 46 and 22 with appreciably distinctive test end times of 12.6 seconds and 21.6 seconds respectively with p-value < 0.001. At 12 week post-operation evaluation, 64% of first group enhanced their function, while 63% of the second group showed pre-operative function. The authors demonstrated that wearable sensors can be integrated with functional examinations during medical visits and that ML can deconstruct multifaceted configurations to disclose clinically pertinent factors.23
A family physician with an expertise in sleep disorders diagnose and manage medical conditions that arise during sleep, that interrupt sleep, or that are disturbed by interruptions in the ‘wake-sleep’ cycle. This specialist is proficient in the evaluation and analysis of polysomnography and administration of a ‘sleep laboratory.’
In 2020, Goldstein et al.’s work summarized a position statement on application of AI in treatment of sleep disorders. The authors foresee that AI’s early application in the sleep medicine facility is the ‘assisted scoring’ of sleep and related incidents through ‘PolySomnoGraphy’ or PSG. They recommend possible medical use cases that excel the ‘sleep laboratory’ and are projected to expand our knowledge of sleep disorders, and therefore improve patients’ health by advancing their sleep care.24
Onyema et al.’s research in 2022 focused on AI modeling of sleep apnea disorder. The data represented 18 patients with apnea syndrome. The AI model demonstrated a substantial association between ECGBP, ECG-EEG, and EEG-BP. The authors determined that the long-term interaction amongst physiological indicators can assist doctors to appreciate the hazards linked with these interactions and aid in detection of obtrusive sleep apnea early.25
A family physician with a specialization in pain medicine identifies and treats people suffering with acuteor chronic pain, or pain related to illness.
In 2021, McGrath et al. work evaluated how in the future AI technology can be integrated in the field of anesthetics. The authors were concerned about how the deep learning models, being built on closed processes, do not offer insights into the connection between input and output data. They worry about if the model were to create “strange” answers in unexpected operating situations. The physicians, in application of anesthetics, do require complete control and therefore will need rule based system.26
Piette et al., in 2022, evaluated if ‘AI’ propelled ‘Cognitive Behavioral Therapy for chronic pain’ or if ‘AICBT- CP’ amplified its efficacy due to patient collaborations. The authors utilized 168 patients based 11,133 ‘AI-CBT-CP’ interactions collected over 10 weeks every week. For each patient, the AI model by optimizing a reward function based on a patient’s pain related information, chose from three treatments: a) a 15 minute live therapy, b) 45 minute live therapy, and c) asynchronous therapist feedback utilizing an ‘interactive voice response’ or IVR call. The reward scores jumped from 0.29 at the start to 0.46 during the 100th week with p-value = 0.002. The authors demonstrated that ‘AICBT- CP’ can acquire from experience what medical management modalities work well to enhance patient results and at the same time preserving doctor’s time.27
In 2021, Salekin et al.’s research focused on AI model to enhance pain management after surgery in neonatal intensive care units (NICU) including minimizing complications. The authors claimed a proactive approach of pain avoidance/minimization intended at precluding harm to newborns from either post-surgical pain or withdrawal due to opioids. Their AI model was built on vital signs, body and facial motions, and incidences of crying to predict ‘time-to-pain’ inception subsequent to post-surgical sedation. This prediction would allow a time period preceding the pain inception for easing with either non-narcotic medicines or non-medicinal mediations.28
Challenges and Opportunities for AI in Family Medicine
There are many obstacles in implementing AI in family medicine which include (a) a readiness of system and data, (b) the possibility for inequity and bias, and (c) the rules of AI. A majority of people do not trust in AI technology, including some of the health providers, as personal connections are more important than computer based tools. Additionally there are major consequences for confidentiality and misuse with utilization of AI. AI by itself could not replace human empathy. In order for AI to be extensively used in family medicine, the family practice physicians need to participate in appropriate plan, strategy, research, and delivery approaches with the technology. Consequently, collaborations between Machine Learning and family practice experts can be effective in both diagnosis and treatment. AI-based technology strengthen family physician’s proficiency and improve patient care, while decreasing treatment costs. However, AI-based diagnosis in family medicine is still not commonly used in clinical practices due to the presence of many legal, privacy, and ethical matters.
Conclusion
AI has the power to magnify clinical efficiency due to its inclination to manage an enormous quantity of data appropriate for automation. However, personal connections are more important than computer based tools. Therefore, in order for AI to be commonly used in family medicine, the family medicine professionals need to partake in its implementation planning, strategy, research, and distribution methods. AI is not going to replace family medicine physicians; instead it can assist family medicine doctors with intuitions that can streamline healing management. AI with the prospective to advance the accuracy of diagnosing different ailments can assist family medicine physicians in delivering appropriate disease recognition and its consequent treatment.
References Références Referencias
1. Kulkarni S., Kulkarni R., Lorenz K. “Artificial Intelligence (AI) in Psychiatry – A Summary.” Global Journal of Medical Research: A Neurology & Nervous System 2022; 22(3): 1-12. Online ISSN:
2249-4618 & Print ISSN: 0975-5888.
2. Buch A., Kulkarni R. “Artificial Intelligence (AI) in Pathology; A Summary and Challenges.” Global Journal of Medical Research, 2021; (K2): 23–34. https://doi.org/10.34257/GJMRKVOL21IS2PG23.
3. Blease C., Bernstein M., Gaab J., et al. “Computerization and the future of primary care: A survey of general practitioners in the UK.” PLoS One. 2018; 13(12): e0207418. doi: 10.1371/journal.
pone.0207418. PMID: 30540791; PMCID: PMC6291067.
4. Summerton N., Cansdale M. “Artificial intelligence and diagnosis in general practice.” Br J Gen Pract. 2019; 69(684): 324-325. doi: 10.3399/ bjgp19X704165. PMID: 31249070; PMCID: PMC6592326.
5. Baser A., BaktırAltuntaş S., Kolcu G., et al. “Artificial Intelligence Anxiety of Family Physicians in Turkey.” Progress in Nutrition 2021; 23(S2): e2021275. https://www.mattioli1885journals.com/index.php/progressinnutrition/article/view/12003.
6. Darcel K., Upshaw T., Craig-Neil A., et al. “Implementing artificial intelligence in Canadian primary care: Barriers and strategies identified through a national deliberative dialogue.” PLoS
ONE 2023; 18(2): e0281733. https://doi.org/10.1371/journal.pone.0281733
7. Liaw W, Kakadiaris I. “Artificial Intelligence and Family Medicine: Better Together.” Fam Med. 2020; 52(1): 8-10. https://doi.org/10.22454/FamMed.2020.881454.
8. Wei W., Tao C., Jiang G., et al. “A high throughput emantic concept frequency based approach for patient identification: a case study using type 2 diabetes mellitus clinical notes.” AMIA Annu Symp Proc. 2010:857-61. PMID: 21347100; PMCID:PMC3041302.
9. Shankaracharya, Odedra D., Samanta S., et al. “Computational intelligence-based diagnosis tool for the detection of prediabetes and type 2 diabetes in India.” Rev Diabet Stud. 2012; 9(1): 55-62. doi:10.1900/RDS.2012.9.55. Epub 2012 May 10. PMID:22972445; PMCID: PMC3448174.
10. Choi DJ., Park J., Ali T., et al. “Artificial intelligence for the diagnosis of heart failure.” npj Digit. Med. 2020; 3: 54. https://doi.org/10.1038/s41746-020-0261-3
11. Hamilton W., Green T., Martins T., et al. “Evaluation of risk assessment tools for suspected cancer in general practice: a cohort study.” Br J Gen Pract. 2013; 63(606): e30-6. doi: 10.3399/bjgp13X660751. PMID: 23336455; PMCID: PMC3529290.
12. “An AI Support Tool to Help Healthcare Professionals in Primary Care to Identify Patients at Risk of Cancer Earlier—NHSX.” 2019 https://www.nhsx.nhs.uk/key-tools-and-info/digitalplaybooks/
cancer-digital-playbook/an- AI-supporttool-to-help-healthcare-professionals-in-primarycare-to-identify-patients-at-risk-of-cancer-earlier/.
13. Kurian B., Trivedi M., Grannemann B., et al. “A computerized decision support system for depression in primarycare.” Prim Care Companion J Clin Psychiatry. 2009; 11(4): 140-6. doi: 10.4088/PCC. 8m00687. PMID: 19750065; PMCID: PMC2736031.
14. Tanguay-Sela M., Benrimoh D., Popescu C., et al. “Evaluating the perceived utility of an artificial intelligence- powered clinical decision support system for depression treatment using a simulation
center.” Psychiatry Res. 2022; 308: 114336. doi:10.1016/j.psychres.2021.114336. Epub 2021 Dec
11. PMID: 34953204.
15. Loskutova N., Lutgen C., Callen E., et al. “Evaluating a Web-Based Adult ADHD Toolkit for Primary Care Clinicians. ”The Journal of the American Board of Family Medicine 2021; 34(4):741-752; DOI: 10.3122/jabfm.2021.04.200606.
16. Nemesure M. Heinz M., Huang R., et al. “Predictive modeling of depression and anxiety using electronic health records and a novel machine learning approach with artificial intelligence.” Scientific report, 2021; 11(1): 1-9. https://doi.org/10.1038/s41598-021-81368-4.
17. Petrauskas V., Jasinevicius R., Damuleviciene G., et al. “Explainable Artificial Intelligence-Based Decision Support System for Assessing the Nutrition-Related Geriatric Syndromes.” Applied Sciences. 2021; 11(24): 11763. https://doi.org/10.3390/app112411763.
18. Vaiyapuri T., Lydia E., Sikkandar M., et al. “Internet of Things and Deep Learning Enabled Elderly Fall DetectionModel for Smart Homecare,” IEEE Access, 2021; 9: 113879-113888. doi: 10.1109/ACCESS. 2021.3094243.
19. Avati A., Jung K., Harman S., et al. “Improving palliative care with deep learning.” BMC Med Inform Decis Mak. 2018; 18(4): 122. doi: 10.1186/s12911-018-0677-8. PMID: 30537977; PMCID:PMC6290509.
20. Wang L., Sha L., Lakin J., et al. “Development and Validation of a Deep Learning Algorithm for Mortality Prediction in Selecting Patients With Dementia for Earlier Palliative Care Interventions.” JAMA Netw Open. 2019; 2(7): e196972. doi: 10.1001/jamanetworkopen.2019.6972. PMID: 31298717;PMCID: PMC6628612.
21. Rigamonti L., Estel K., Gehlen T. et al. “Use of artificial intelligence in sports medicine: a report of 5 fictional cases.” BMC Sports Sci Med Rehabil. 2021; 13: 13. https://doi.org/10.1186/s13102-021-00243-x.
22. Novatchkov H., Baca A. “Artificial Intelligence in Sports on the Example of Weight Training.” Journal of Sports Science and Medicine 2013; (12): 27-37.https://www.jssm.org/jssm-12-27.xml%3EFulltext#.
23. Bloomfield R., Williams H., Broberg J., et al. “Machine Learning Groups Patients by Early Functional Improvement Likelihood Based on Wearable Sensor Instrumented Preoperative Timed-Up-and-Go Tests.” The Journal of Arthroplasty, 2019; 34(10): 2267-2271. ISSN 0883-5403, https://doi.org/10.1016/j.arth.2019.05.061.
24. Goldstein C., Berry R., Kent D., et al. “Artificial intelligence in sleep medicine: an American Academy of Sleep Medicine position statement.” J Clin Sleep Med. 2020; 16(4): 605–607. https://jcsm.aasm.org/doi/10.5664/jcsm.8288.
25. Onyema E., Ahanger T., Samir G., et al. “Empirical Analysis of Apnea Syndrome Using an Artificial Intelligence- Based Granger Panel Model Approach.” Computational Intelligence and Neuroscience, 2022. Article ID 7969389. https://doi.org/10.1155/2022/7969389
26. McGrath H., Flanagan C., Zeng L., et al. “Future of Artificial Intelligence in Anesthetics and Pain Management.” Journal of Biosciences and Medicines, 2019; 7: 111-118. https://doi.org/10.4236/jbm.2019.711010.
27. Piette J., Newman S., Krein S., et al. “Artificial Intelligence (AI) to improve chronic pain care: Evidence of AI learning,” Intelligence-Based Medicine, 2022; 6: 100064. ISSN 2666-5212. https://doi.org/10.1016/j.ibmed.2022.100064.
28. Salekin M., Mouton P., Zamzmi G., et al. “Future roles of artificial intelligence in early pain management ofnewborns.” Paediatr Neonatal Pain. 2021; 3: 134–145. https://doi.org/10.1002/
pne2.12060.

