I. Introduction
The key goal of this paper is to evaluate applications of Artificial Intelligence (AI) and machine learning in the field of psychiatry. The past thirty years have shown rapid progress in the use of AI to medical images based fields of radiology, neurology, pathology, and ophthalmology. In addition, as shown in Figure 1, AI has been an essential tool in various medicine-related applications.
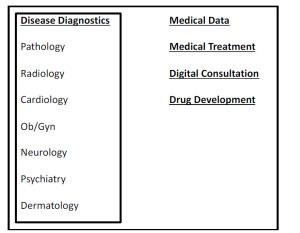
Figure 1. AI in medicine
In the field of psychiatry, as shown in Figure 2, AI has applications in disease determination, categorizing various psychiatric conditions, and various mood disorders.
| Adult psychiatry
Old age psychiatry Children/adolescent psychiatry Addiction psychiatry Forensic psychiatry Learning disability |
Figure 2. AI in psychiatry
In this article, first we reviewed Artificial Intelligence-based psychiatry research in various clinical situations that are included in Figure 2. Secondly, different ethical and social issues of AI Artificial Intelligence faces for use in psychiatric applications are discussed.
II. Artificial Intelligence or AI
By definition, Artificial Intelligence or AI is an intelligence that is not natural or is artificial. AI is founded on various statistical principles where a phenomenon is ‘learned’ by a machine. The phenomenon gets cleverer as more learning of it is managed. After a suitable quantity of this training, then, AI can be, as a human being, useful for making decisions. In this section important AI terms and ML-based algorithms are explained.
- AI basics
In this section, important AI terms are briefly discussed.Machine learning (ML) approach pools statistical modeling and computers together to learn from available data. ML is characterized into ‘supervised’ and ‘unsupervised’ learning.- Supervised learning method builds a forecast model of a known output and input data set. The model is then utilized to predict new output given new output information. This approach is well suited for both i) ‘classification’ model for output categories (e.g., a patient has an illness or patient does not is based on an MRI scan) and ii) ‘regression’ model where the output variable is continuous (e.g., patient’s weight).
- Unsupervised learning approach groups data together, to comprehend the intrinsic structure of the data, based on their resemblances and when there is no output prediction variable and input data is not labeled. E.g., clustering patterns in a sample of patients with an illness that could lead to new drug therapy.
- Semi-supervised learning is a blend of ‘Supervised’ and ‘Unsupervised’ learning approaches (e.g., conglomerate algorithms of ‘classification’ and ‘clustering’)Artificial Neural Networks or ANNs attains an output forecast that results from numerous independent phases of computations and weightings. ANN, similar to a neuron network in a brain, has a set of artificial layered/connected neurons to transfer data through the web.
- ML algorithms
Supervised Machine Learning modeling involves the splitting the available information into both ‘training’ (or ‘educating’) and ‘testing’ data sets for verification. In Supervised ML, the following algorithms are extensively utilized:- Regression: For ML, both ‘Linear regression’ (use of least squares regression line with the lowest error among the cause/independent variables and the effect/dependent variables), and ‘Logistic Regression’ (used for binary outcomes of ‘yes/no,’ or ‘no illness/illness’ with forecasters types of either categorical or continuous) methods are commonly used based on data characteristics.
- Decision Tree (DT): The decision tree-based ML algorithm includes a set of rules that describes the pathway from the root to the leaves. The feature of interest is analyzed at the node while the output of the analysis is assigned at the branch.
- Naive Bayes: ML algorithm based on Naive Bayes postulates that the characters under assessment are independent of each other.
- Support Vector Machine (SVM): The Support Vector Machine-based ML algorithm finds a nonlinear relationship and categorizes data by describing a hyperplane that best distinguishes the existence of two groups.
- k-Nearest Neighbor (k-NN): ‘k-Nearest Neighbor’ based ML algorithm is utilized for data categorization of nonparametric grouping. The ‘k’ is defined as the square root of the number of incidences and its remoteness from a pre-selected point. Moreover, the categorization is established on the number of k neighbors.
- Random Forest (RF): ML with Random Forest algorithm, which prevents ‘overfitting,’ is an efficient tool for an accurate estimate of classifiers. Nevertheless, the RF-based ML algorithms are less proficient than the SVM/or k-NN/logistic regression-based ML methods.
- Convolutional Neural Networks (CNNs): ‘Convolution’ is a form of a mathematical function on two functions that produces a third function. Convolutional Neural Networks, feed-forward networks, learn by using numerous layers of nodes and several replications of both ‘analyzing’ and ‘weighting’ the patterns it recognizes in the images. The value/size of weights is decided based on how correctly it classifies a design or structure.
- AI in mood disorders
Health professionals use ‘mood disorder,’ a mental health category, to generally label all categories of depression and bipolar disorders. However, a significant overlap in symptoms exists between these disorders. This is where AI and machine learning come into play with their potential to improve the accuracy of diagnosing different mood disorders.- AI in depression
Having less concern in everyday activities, feeling unhappy or miserable, and other similar indications for minimum two weeks may signal depression.
In 2020, Richter et al. research focused on a novel methodology to assess for dissimilarities in cognitive prejudices amid subclinical depressed and anxious persons. They, based on the stages of depression and anxiety indications, separated 125 people into four groups. A wide-ranging behavioral examination sequence revealed and measured numerous ‘cognitive–emotional’ biases. The authors developed sophisticated machine learning (ML) tools to scrutinize these outcomes. These techniques uncovered distinctive configurations that differentiate depression against anxiety. The model distinguished well between symptomatic members (with high signs of depression, anxiety, or both anxiety) compared to the control group with no symptoms. It resulted in a 71.44% classification prediction accuracy (sensitivity) for ‘high anxiety/high depression/high anxiety and high depression’ and 70.78% classification prediction accuracy (specificity) for ‘low anxiety and low depression.’ In addition, the model yielded in classification prediction accuracy of 68% for ‘high depression’ while 74.18% for ‘high anxiety.’1Li et al. in 2019 used electroencephalogram (or EEG to detect electrical activity in the brain using small, metal electrodes attached to the patient’s scalp) and ML to better diagnose depression amongst 28 individuals. The Mini-International Neuropsychiatric Interview (MINI) approach was utilized by the physicians as the measure by the authors for the identification of depression. Original features of ‘power spectral density’ and ‘activity’ were individually obtained by means of auto-regress model’ and the Hjorth algorithm with specific time frames. Two distinct methods of ‘ensemble learning’ and ‘deep learning’ processed these features. The ensemble learning used a deep forest transformation of the original features to new and a support vector machine (SVM) as a classifier. In the deep learning method, the authors added spatial data of EEG caps to both features and implemented Convolutional Neural Network (CNN) for recognition. Their approach yielded accuracy of 89% using the ensemble model and power spectral density. The deep learning method achieved 84.75% accuracy using the activity. The research showed that EEG could be utilized as a dependable gauge for recognizing depression.2In 2018, Dinga et al.’s work assessed the predictive value of a varied range of clinical, biological, and psychological features for forecasting the progression of depression and targeted to detect the top predictors. The authors evaluated 804 patients with dysthymia or unipolar depression involving 81 of these features. The patients were clinically monitored for two years. The patients, applying a latent class growth analysis, were grouped into (i) the presence or lack of a depression, and (ii) disease course trajectory groups of rapid remission, gradual improvement, and chronic. The authors used a ‘penalized logistic regression’ to forecast depression progression and to also assess the predictive magnitude of distinct variables. They, established on the inventory of depressive symptomatology (IDS), estimated a swift reduction course of depression with an area under the Receiver Operating Characteristic (ROC) curve of 0.69 with 62% accuracy. Also, at follow-up, the existence of an MDD identification presented an area under ROC of 0.66 and 66% accuracy. Out of the sizeable set of considered parameters, only the IDS offered prognostic magnitude for course forecast on an individual level. Though the accuracy of course prediction was moderate at best.3Chekroud et al. in 2016, came up with a procedure to evaluate whether patients with depression will attain symptomatic reduction from a twelve-week treatment of an antidepressant such as citalopram. The authors used self-reported data from 1,941 patients with depression from ‘ClinicalTrials.gov’ (number NCT00021528) to detect variables with the highest predictive of medical treatment results. They utilized these variables for training an ML model to forecast clinical depression remission. This model was externally confirmed by them in the escitalopram treatment group of 151 patients from a separate clinical trial (number NCT00590863). The ML model was trained with 25 self-reported variables, with the most predictive of treatment outcome, from 164 patients. The model, after internal cross-validation, predicted outcomes with an accuracy of 64·6% with p<0·0001. The external validation of the 151 patients from the escitalopram treatment group attained an accuracy of 59·6% with p=0.043. The model, when applied to a combined escitalopram-bupropion treatment group of 134 patients, resulted in an accuracy of 59·7% with p=0·023. However, when used for a combined venlafaxine-mirtazapine group of 140, the model displayed an accuracy of 51·4% with p=0·53, suggesting the model’s specificity to core mechanisms. The authors showed that use of the ML models by extracting available clinical test data can allow potential identification of patients prone to have a positive response to a specific antidepressant.4In 2015, Patel et al., for accurate diagnosis and treatment of depression, studied numerous ML approaches with
‘multi-modal imaging’ and ‘non-imaging’ whole brain and network-based features as inputs. The authors recruited 33 older depressed and 35 late-life non-depressed individuals. Their demographics and cognitive ability scores were first documented, followed by attainment of their brain characteristics using multi-modal MRI. Linear and nonlinear ML methods were then examined by the authors for appraising models’ predictive accuracy. An ‘alternating decision trees’ method projected the highest accurate forecast models for late-life depression diagnosis with 87.27% accuracy, while the treatment response attained 89.47% accuracy. The diagnosis model included measures of age, Mini-mental state examination score, and structural imaging (e.g., whole brain atrophy and global white mater hyperintensity burden). The treatment response model included measures of structural and functional connectivity. Thus multi-modal imaging coupled with a ‘non-imaging’ methods-based approach can predict depression diagnosis and treatment response for older age patients and allow custom-made depression treatment for them.5In 2013, Hosseinifard et al.’s work demonstrated, based on 45 un-medicated depressed patients and 45 normal subjects, that nonlinear analysis of EEG is valuable method for discerning depressed patients and control subjects. From the EEG signal, the authors extracted four nonlinear features (Lyapunov exponent, Higuchi fractal, detrended fluctuation analysis, and correlation dimension. For differentiating the two groups, the authors, as the classifiers, used ‘k-nearest neighbor,’ ‘linear discriminant analysis’ and ‘logistic regression.’ The highest classification accuracy of 83.3% was achieved by correlation dimension and LR classifier. The authors improved their model when all nonlinear features were collectively applied to classifiers yielding a classification accuracy of 90% by LR classifier and all nonlinear features.6 - AI in bipolar disorders(BD) and schizophrenia (SZ)
Bipolar disorder is a circumstance when a person has phases of depression interchanging with phases of raised mood or mania. In comparison, an individual with schizophrenia interprets reality abnormally and has two or more symptoms out of: delusions, hallucinations, disorganized speech, grossly disorganized or catatonic behavior, and negative symptoms.
Tomasik et al. in 2021, based on blood biomarker data and an online questionnaire, developed a diagnostic algorithm to decrease the misidentification of ‘Bipolar Disorder’ (BD) as ‘Major Depressive Disorder’ (MDD). Their model utilized data from patients aged 18-45 years with depressive symptoms. In order to establish their depression diagnosis, phone interviews were conducted after patients answered an online questionnaires and provided dried blood samples for biomarker assessment. The authors applied ‘Extreme Gradient Boosting’ followed by nested cross-validation to train and validate models distinguishing BD from MDD in individuals who self-described diagnosis of MDD. The area under the ROC curve for splitting participants with ‘BD diagnosed as MDD’ from those with ‘truthful MDD’ was 0.92 with a 95% Confidence Interval of 0.86–0.97. Validation in cases of participants without previous diagnosis of mood disorder diagnosis produced area under the ROC of 0.89 and 0.90 for distinguishing newly identified BD and subclinical low mood from MDD, respectively. Validation in participants with previous BD identification showed 86% sensitivity. The authors’ algorithm thus accurately recognized patients with BD in numerous clinical circumstances, which could assist in accurate clinical identification and management of BD.7n 2021, Siqueira Rotenberg et al.’s research analyzed ML approaches as a likely forecaster in BD-related depressive relapses. The authors applied ML algorithms of RF, SVM, Multilayer Perceptron, and Naïve Bayes, to a group of 800 patients (507 with depressive relapses and the remaining 293 without). The ML algorithms’ prediction ranged between 61 and 80% in terms of F-measure. The RF approach’s performance was the best, with 68% for a relapse cohort and 74% without. Thus, ML algorithms can assist in clinical decision-making for patients requiring BD management.8Fernandes et al. in 2020, using immune and inflammatory biomarkers in peripheral blood and cognitive biomarkers utilizing ML, established a model with probabilistic multi-domain data integration in order to predict the identification of BD and schizophrenia (SZ) based on 416 participants. Their model for ‘with the BD’ vs. ‘without’ displayed a sensitivity of 80% and specificity of 71%. For ‘ with the SZ’ vs. ‘without’, the model produced sensitivity and specificity of 84% and 81%, respectively. However, the model was moderately effective for the discriminating between BD and SZ with a sensitivity of 71% and specificity of 73%.9In 2019, Belizario et al. work focused on understanding if Predominant polarity (PP) is a vital specifier of BD. The authors applied ML algorithms to establish a patient´s PP but without including the number and polarity of past incidents, and searched for the links between PP and demographic/clinical factors. Clinical and demographic characteristics were gathered from 148 BD patients using a tailored questionnaire. The authors utilized the RF algorithm to categorize patients into either ‘depressive’ or ‘manic’ PP and uncover which factors were linked to the specifier.
The model produced an area under the ROC curve of 74.72% in categorizing patients into either ‘depressive’ or ‘manic’ PP. The top factors selected by the model included: age at the first depressive episode, number of hospitalizations, BD Type II, manic onset, and delusions. Additionally, anxiety disorders, alcohol dependence, eating disorders, and substance dependence appeared to be linked with PP. The research work demonstrated that the ML could assist in a patient’s PP diagnosis.10In 2018 Perez Arribas et al. applied a ‘signature-based’ learning method to a cohort of 130 participants (48 with BD, 31 with borderline personality disorder, and 51 control) who, using a bespoke smartphone app, daily submitted for one-year mood ratings. The model was used to record the progressing interrelations amongst the distinctive features of mood and use this information to categorize participants’ diagnosis and to forecast succeeding mood status. The model could differentiate amongst the three participant cohorts, with categorization accuracy of classified 75% into the correct diagnostic cohort versus with 54% utilizing standard methods. Additionally, succeeding mood scores were accurately forecasted with higher than 70% accuracy. The forecast of mood was most accurate in the control group (89–98%), followed by bipolar disorder (82–90%) and borderline personality disorder (70–78%). The authors thus successfully demonstrated the signature method to analyze mood data in terms of diagnostic classification and prediction of future mood.11Schnack et al. in 2014 work focused on utilizing MRI scans to distinguish SZ from BD. Their study included scans, using a 1.5 T MRI scanner, of 198 participants (66 each with SZ, with BD, and the healthy/control). Three SVMs, based on their gray matter density images, were trained to distinguish patients with SZ from the control group, patients with SZ from those with BD, and patients with BD from the control cohort. The model separated a) SZ patients from BD patients with an accuracy of 88%, and b) patients with SZ from control participants with an accuracy of 90%. The approach was moderately accurate is separating BD patients from the control cohort with correct categorization (accuracy for BD 53% and control 67%). Application of 1.5 T MRI scanner-based models on a validation set from a 3 T MRI scanner provided average categorization accuracies of 76% (control vs. SZ), 66% (BD vs. SZ), and 61% (control vs. BD). This research work, based on structural MRI scans, showed that the accurate separation of SZ from BD using gray matter pathology caould aid in the differential diagnosis of these disorders.12 - AI in suicidality with mood disorders
Suicide, an individual taking their own life, is a catastrophic response to traumatic life circumstances. A majority of all suicides are by individuals who agonize from mood disorders. Thus, avoidance of suicide among those who suffer from mood disorders is a key to preventing a suicide.
In 2021 Hong et al.’s research assessed a group of 66 adolescents and young adults with MDD diagnosis. They obtained T1-weighted MRI scans which then were categorized utilizing the SVM algorithm to separate ‘suicide attempters’ from people with ‘suicidal ideation but without attempts.’ Their model identified ‘suicide attempters’ and individuals with ‘suicidal ideation but without attempts’ with an accuracy of 78.59%, the sensitivity of 73.17%, and specificity of 84.0%. For the ‘suicide attempters,’ the Positive Predictive Value (PPV) of suicide attempts was 88.24%, while the Negative Predictive Value (NPV) was 65.63%. The authors were able to derive the top 10 ranked classifiers for a suicide attempts. The outcomes of this research specified that structural MRI-based information could be beneficial for the categorization of suicide possibility among MDD patients.13Agne et al. in 2020 work focused on understanding the reasons why patients with obsessive-compulsive disorder (OCD) have a higher risk of suicide attempts vs. the general population. The authors used the ML method to find out if the driver(s) of the higher suicide attempts include the sociodemographic factors and comorbidities. The analysis included 959 patients with OCD using an elastic net model to identify the forecasters of suicide attempts utilizing sociodemographic and clinical factors. The occurrence of suicide attempts in the sample authors studied was 10.8%. The model yielded a) previous suicide planning, b) previous suicide thoughts, c) lifetime depressive episodes, and d) intermittent explosive disorder as relevant predictors of suicide attempts. The elastic net model with an area under the curve of 0.95 thus provided a high accuracy performance algorithm.14In 2019, Carson et al. developed a ML algorithm utilizing natural language processing of electronic health records to detect suicidal conduct among youths those are hospitalized for psychiatric issues. A total of 73 individuals from the northeastern US, with an electronic health record, available before hospitalization, who responded to a survey for a record of suicide attempts in the past year before the hospitalization were selected for this study. The clinical notes from these records prior to inpatient admission were processed for phrases linked with the suicide attempt. The authors then applied the RF machine learning approach to develop a categorization model. The model demonstrated i) a sensitivity of 0.83, ii) specificity of 0.22, iii) area under the curve of 0.68, iv) a PPV of 0.42, v) NPV of 0.67, and vi) an accuracy of 0.47. The phrases highly linked with suicide attempts are grouped around terms related to suicide, psychotropic medications, psychiatric disorders, and family members. This research thus displayed a reasonable achievement of a natural language processing method in the identification of suicide attempts among hospitalized youths with a psychiatric background.15In 2017, Jihoon et al.’s work focused on if the data from multiple clinical scales have categorization power for detecting actual suicide attempts. Five hundred seventy-three participants with disorders of depression and anxiety completed questionnaires, including 31 psychiatric scales, concerning their record of suicide attempts. The authors first trained an ANN classifier with total of 41 factors (31 psychiatric scales and ten sociodemographic factors), followed by a ranking of the impact of each factor on the categorization of suicide attempts. The model demonstrated an accuracy of detecting suicide attempts of 94% in one month, 91% in one year, and 87% in a lifetime. The areas under the ROC curves for suicide attempts detection were 0.93 for one month, 0.87 for one year, and 0.89 for a lifetime. The questionnaire regarding ‘Emotion Regulation’ had the highest impact among all factors. This ML-based research thus demonstrated that self-reported clinical scales could be valuable for the categorizing of suicide attempts.16Passos et al.’s study in 2016 looked at various clinical risk variables to calculate the likelihood of an individual attempting suicide. Demographic and clinical variables based data from 144 patients, who were diagnosed with a mood disorder, was used for training an ML algorithm. This algorithm was then used by the authors in classifying new individuals as either ‘suicide attempters’ or ‘non-attempters.’ Three different ML algorithms were applied and assessed. All these algorithms separated ‘suicide attempters’ from ‘non-attempters’ with forecast accuracy ranging from 65% to 72% with p value < 0.05. The Relevance Vector Machine (RVM) algorithm correctly forecasted the behavior of 103 of the 144 subjects producing 72% accuracy and an AOC of 0.77 with a p-value < 0.0001. The critical predictor factors in discriminating ‘suicide attempters’ from ‘non-attempters’ comprised of a) prior hospitalizations for depression, b) a record of psychosis, c) cocaine dependency, and d) posttraumatic stress disorder. Thus, the authors were able to identify demographic and clinical risk factors for suicide attempts in individuals with mood disorders.17 - AI in Addiction
Despite harmful consequences, uncontrolled consumption of either a substance (e.g., drugs, alcohol, food) or a medium (e.g., technology). The person’s capacity to function in day-to-day life can become compromised with addiction even though the individuals know the habit is producing or will produce complications.
In 2021, Gao et al.’s study focused on a ‘proteome-informed’ ML algorithm to uncover an almost ideal compounds for anti-cocaine dependence. The authors using 32 ML different models, performed over 60K experimental drugs for side effects and re-purposing possibilities. All of the current drug candidates did fail in both cross-target and Absorption/Distribution/Metabolism/Excretion/Toxicity (ADMET) screenings. However, the ML algorithms recognized numerous ‘nearly optimum’ possibilities for additional optimization.18Choi et al.’s research in 2021aimed to categorize predictor factors (e.g., environmental causes,
social, and mental) that produce nicotine dependence in youth who consume e-cigarette or hookah consumers and construct nicotine dependence forecast models using ML algorithms of a) RF with ReliefF and b) Least Absolute Shrinkage and Selection Operator or LASSO. These ML-based prediction models utilized data from the 2019 National Youth Tobacco Survey participants of 6,511 who were recognized as ever consumed either e-cigarettes or hookah. A final analysis based on 193 predictor factors showed a) witnessed e-cigarette use in their household, and b) perception of their tobacco use as top factors that could be utilized in public alertness for policymakers.19In 2021 Wang et al.’s work focused on developing SVM models to recognize internet addiction and evaluate the effectiveness of cognitive behavior therapy (CBT) founded on ‘unbiased functional connectivity density or FCD.’ Total of 57 participants (27 with IA and 30 with healthy control or HC) provided resting-state fMRI before and after eight-week CBT meetings. The discriminatory FCDs were calculated as the characters of the support vector classification model to identify persons with IAs from the HCs. The authors’ model effectively separated participants with IA with an accuracy of 82.5% from HCs with an area under the curve of 0.91. Furthermore, FCDs of potential neuroimaging biomarkers for IA were confirmed as a) hyperactive-impulsive habit system, b) hypoactive-reflecting system, and c) sensitive interoceptive reward awareness system.20In 2019, Symons et al.’s research efforts analyzed the performance of ML models vs. medical professionals to forecast alcohol addiction results in patients after CBT. Twenty-eight ML models were built and trained utilizing a) demographic and b) psychometric assessment data from 780 patients who had gone through a 12-week, abstinence-based CBT program for alcohol addiction. Additional 50 patients for prediction were assessed by i) ten addiction therapy experts, and with ii) twenty-eight trained ML models. The highest accuracy ML model of 74% was far superior vs. the four least accurate therapists, with 51% to 40% accuracy. However, the model’s robustness was low as the area under the ROC curve was only 0.49. The mean aggregate predictive accuracy of these 28 ML models was slightly better (58.6%) than the ten clinical therapists (56.1%). Thus the research showed that the highest performing prediction models have the potential to help the therapists in clinical settings.21 - AI in forensic psychiatry
Forensic psychiatry tends toward a heavy emphasis on science, and forensic psychiatrists identify and handle mental disorders in the framework of the criminal judicial system.
In 2022, Hoffmann et al., using ML methods, explored aggression in 370 offender inpatients with schizophrenia spectrum disorders (SSDs). The SVM based models yielded the best accuracy out of all ML models, with an accuracy of 77.6% and an area under the ROC curve of 0.87. The most predictive factors in separating ‘aggressive’ from ‘non-aggressive’ in inpatients were a) negative behavior toward other patients, b) the breaking of ward rules, c) the positive and negative syndrome (PANSS) score at admittance, d) poor impulse control and impulsivity. This research is a good example of ML’s usefulness in forensic psychiatric research related to aggression in SSD.22In 2021 Watts et al. applied ML techniques to predict the type of criminal wrongdoings in psychiatry patients, at an individual level. Multiple ML models (Random Forest, Elastic Net, SVM) were built and trained based on 1,240 patients in the forensic psychiatric health system. Using only 36 clinical factors, sexual crimes were forecasted by the authors, from both ‘non-violent’ and ‘violent’ offenses with a sensitivity of 82.4% and specificity of 60.0%. The authors, utilizing a binary classification model with 20 clinical factors, forecasted sexual and violent acts, with 83.3% sensitivity and 77.4% specificity. Furthermore, using 30 clinical factors, non-violent and sexual offenses can be separately forecasted with 74.6% sensitivity and 80.7% specificity. These results indicate that ML models can display higher accuracy than the current risk assessment tools (which also cannot individually predict) with the area under the ROC curves between 0.70 and 0.80. However, a considerable subset of patients in this analysis had a history in the criminal system preceding an official diagnosis. Thus, many of the factors that forecast these behaviors might result from the problems of past offenses.23Philipp et al., in 2020, using ML, investigated 569 predictor factors for their forecasting power for either ‘coercion’ or ‘no coercion’ in 358 patients (131 who did experience coercion while 227 who did not). The data was split
(70/30%) first to find the best ML model (70% of data) and the remainder data (30%) for extracting most essential factors from the best model found. The best model had a balanced accuracy of 73.3% and an area under the ROC curve (a predictive power) of 0.85 with the top five prediction factors of a) threat of violence, b) actual violence toward others, c) the application of direct coercive measures during past psychiatric inpatient treatments, d) the PANSS poor impulse control, e) uncooperativeness, and hostility. This research confirmed prior discoveries and added detail on variables revealing the use of coercion.24 - AI in personality disorders
Kinds of personality disorders are categorized into three groups/clusters, founded on similar features and indications. These personality disorders are:
a) Cluster A is categorized by odd, eccentric thought processes and, or conduct,
b) Cluster B is categorized by the overly emotional thought processes and, or unpredictable conduct,
c) Cluster C is categorized by anxious, fearful thought processes and, or conduct.In 2014, Randa et al. built an ‘expert system,’ which mimics the ‘expert rational’ in deciphering a problem, of personality disorders to help assist in the early identification of the illness. The authors used a ‘Certainty Factor’ method to estimate the likelihood of someone is suffering from this illness. They demonstrated an approach to establishing the types of personality disorders founded on symptoms experienced. Their calculations based on the method of Certainty Factor displayed a 77.2% confidence level.25Berdahl, in 2010, developed a framework for etiology of Borderline Personality Disorder (BPD) by building a NN with restrictions from a) neuroanatomy, b) neurophysiology, and c) behavior. The NN models showed how various brain make-ups could interrelate during BPD. These NN simulations indicated that long-term depression (LTD) in the brain structures might clarify various BPD symptoms.26Hayat et al. in 2019 investigated a back propagation neural network (BPPN) model for the early discovery of type B personal disorder. The model used 43 data points for training and 34 for testing. The model’s output was cataloged into four identification classifications of type B personal disorder: i) anti-social, ii) borderline, iii) histrionic, and iv) narcissistic. The model achieved an accuracy of 90.7% in training and 97.2% in testing. The authors thus showed a high accuracy BPPN model to diagnose type B personal disorder.27 - AI in child and adolescent psychiatry
The child and adolescent psychiatric fields focus on the identification and the management of disorders of
i) thinking, and ii) feeling and, or behavior disturbing children, adolescents, and their families.In 2022 Dobias et al. utilized individual sociodemographic factors and depression symptoms as predictors to study the capacity to forecast ‘whether’ and ‘where’ adolescents (ages 12-17) get mental healthcare. The authors analyzed data from the 2017 National Survey of Drug Use and Health as a characteristic sample of non-institutionalized individuals in the US. The analysis included both RF and elastic net-based ML models. The model’s assessment was based on data from total of 1,671 youths (inpatient, outpatient, and other) with raised depressive symptoms. Only 53% of these youths sought care of any kind. Using the two predictors, the RF models explained no ‘pseudo- out-of-sample’ deviance in youth accessing any depression treatment, while elastic net models performed slightly better, explaining 0.80–2.50% ‘pseudo-out-of-sample’ deviance for access to all depression treatments. This research thus showed considerable limits in our ability to forecast ‘whether’ and ‘where’ youths access mental healthcare.28Haque et al.’s research in 2021focused on ML algorithms for detecting depression among children and, or youths aged four to17 years and factors that contribute to the illness. In this research, for modeling, multiple available datasets from 2013-14 for the Australian children and youths were used. In the depression recognition step, MF algorithms based on RF, XGBoost, Decision Tree, and Gaussian Naive Bayes were used. The RF-based ML algorithm was the best in forecasting depressed categories by 99% with an accuracy of 95%.29In 2021, Price et al. studied the association between childhood maltreatment and structural alterations in the brain. They utilized ML based on elastic net regularized regression to detect if and how brain structure differed among young adults (18-21 years of age) with and without a record of mistreatment. A total of 384 individuals completed an evaluation of juvenile trauma experience and a structural MRI. A model which included five subcortical volumes, seven cortical thicknesses, and 15 surface areas yielded an area under the ROC curve of 0.71 with a p-value less than 0.001. The individuals with a mistreatment past had smaller surface areas and cortical thicknesses predominantly in ‘frontotemporal’ areas. They also displayed more enormous cortical thicknesses in occipital regions and larger surface areas in frontal regions. This research clearly demonstrated that childhood abuse is associated with numerous measures of structure in the brain.30To diagnose anxiety and depression, McGinnis et al. in 2018 proposed the application of a 90-second fear induction task during which time an individual’s motion is monitored using a wearable sensor that is commercially available. In contrast, current diagnostic approaches for detecting the illness takes days. A multitude of ML models was utilized by the authors to extract from one 20-second phase of the task to forecast diagnosis. The best model demonstrated a diagnostic accuracy of 75%, comparable to current diagnostic methods, however, at a relatively insignificant fraction of the time and cost.31In 2017 Saxe et al. studied if ML methods can generate predictive categorization models for childhood Posttraumatic Stress Disorder (PTSD) and also if explicit factors can be recognized for the disorder. The authors applied ML forecasting categorization methods to 105 biopsychosocial risk variables. The variables were based on data which was collected from 163 injured hospitalized children that were diagnosed with PTSD three months after their discharge. A forecasting categorization model was realized by the authors with meaningful accuracy. A model built based on subsets of possibly causally relevant characters achieved similar forecasting ability paralleled to the best model constructed with all factors. The authors found that the Causal Discovery Character Choice-based methods recognized 58 factors, of which ten were classified as very stable. Thus authors using ML algorithms could establish both forecasting categorization models for childhood PTSD and categorize numerous causal factors.32 - AI in attention deficit hyperactivity disorder (ADHD)
An individual with attention deficit hyperactivity disorder (ADHD) condition has differentiations in brain development and brain activity, from a normal brain, which disturbs attention, the ability to sit static, and self-discipline. It is critical to diagnose children with displaying substantial losses and symptoms of ADHD at an early age as early detection and treatment may lead to more effective, and shorter treatment.In 2011, Delavarian et al. explored the use of AI in diagnosing children with different behavioral disorders. By using the Matlab toolbox for pattern recognition known as “Prtools,” the authors examined a total of 16 different classifiers and their accuracies in differentiating between childhood conditions that present with similar symptoms. The specific disorders included ADHD, depression, anxiety, comorbid depression and anxiety, and conduct disorder (i.e., the outputs). The study involved 306 children, and 38 common symptoms of childhood behavioral disorders were used as inputs. The authors concluded, from the data collected, that the nearest mean classifier was the most accurate classifier, with an accuracy of 96.92%. Not only was it the most accurate of the classifiers examined, but it was also significantly more accurate in diagnosing children with behavioral disorders compared to not using a classifier at all (87.51%). The authors showed that the use of specific classifiers can help aid in improving the correct diagnosis of childhood behavioral disorders. This is key, as correctly identifying patients with these disorders at earlier stages in life will allow for earlier interventions and subsequently improved outcomes.33In 2010, Anuradha et al.’s research applied the SVM Algorithm in diagnosing ADHD. The Support Vector Machines are a frequently utilized artificial intelligence technique; by constructing a hyperplane or sets of hyperplanes in a high-dimensional space, the authors used this technique to classify a group of 100 children, ages 7-10 years old, as either having or not having ADHD. The input to the SVM Algorithm was primarily in the form of answers to a questionnaire. The questionnaire consisted of 6 yes-or-no questions, with values of 1 given to “yes” answers and 0 assigned to “no” answers. After the input data was fed into the Algorithm, the output was recorded as either “1” for diagnosis of ADHD or “0” for no diagnosis of ADHD. According to the data reported in this study, the SVM Algorithm was correct in diagnosing/not diagnosing ADHD 88.7% of the time when comparing the output from the Algorithm to the diagnoses made by trained physicians. (While this study design assumes that the physicians are correct in their diagnoses, it is promising that this Algorithm can match the diagnosis of trained physicians nearly 90% of the time).34Ariyarathne et al. in 2020, based on a CNN model, proposed using fMRI data of the “resting brain” in conjunction with seed-based correlation analysis to classify and identify children with ADHD. Seed-based correlation analysis works by computing the functional connectivity between different regions within the brain. Four specific brain regions were studied, including the Medial Prefrontal Cortex (MPC), Posterior Cingulate Cortex (PCC), Left Temporoparietal Junction (LT), and Right Temporoparietal Junction (RT). From the seed-based correlation analysis of these brain regions, a Convolution Neural Network (CNN) was used as a pattern recognition classifier to distinguish between patients with ADHD and patients without ADHD (controls). According to the results, the accuracy of classification of patients with ADHD was highest in the Medial Prefrontal Cortex (MPC) region of the brain at 85.21%. This should not come as a surprise, claimed the researchers, as the primary region of the brain implicated with ADHD is the prefrontal cortex.35 - AI in geriatric psychiatry
Geriatric psychiatry, the practice of psychiatry in older adults, is a vital field of psychiatry. Many of aging related body changes (e.g., blood and nervous system) might escalate an individual’s probability to suffer depression, mental impairment, and dementia. In 2021 Yadgir et al.’s study focused on ways to categorizing patients, aged above 59 years, with a high risk of Cognitive Impairment (CI) using ML-based on factors accessible from electronic health records (EHRs). The authors used records of 1,736 adults who were dismissed from three emergency departments (EDs). Each adult’s CI was estimated by the authors, based on the ‘Blessed Orientation Memory Concentration’ (BOMC) test conducted in the ED. A ‘nested cross-validation’ framework was utilized to assess ML algorithms. Using BOMC scores, 121 (7% of 1,736) adults tested positive for potential CI. The top-performing ML algorithm, of XGBoost, forecasted BOMC positivity with an area under the ROC curve of 0.72. With a categorization threshold of 0.4, the model yielded 0.73 sensitivity, 0.64 specificity, an NPV of 0.97, and a PPV of 0.13. This work showed that an ML algorithm built on EHR data could separate patients at higher risk for CI.36Hemrungrojn et al., using a neural network algorithm, in 2021, looked at the Thai population for the categorization of amnestic mild cognitive impairment (aMCI) and Alzheimer’s disease (AD). The authors used Montreal Cognitive Assessment (MoCA) to study incorporated 60 AD patients, 61 aMCI patients, and 60 healthy controls (HCs). The authors, using their model, discriminated against aMCI patients from AD patients with an area under the ROC curve of 0.94, and HC with an area under the ROC curve of 0.81. The ML method exhibited that i) ‘aberrations in recall’ was the most significant feature of aMCI vs. HC, and ii) ‘aberrations in visuospatial skills’ and ‘executive functions’ were the top features of AD versus aMCI. Furthermore, impairments in a) recall, b) language, and c) orientation distinguished AD from aMCI. However, d) attention, e) concentration, and f) working memory did not. Thus the authors demonstrated that the ML algorithm based on ‘MoCA’ is a suitable cognitive assessment tool for the Thai population for the identification of aMCI and AD.37In 2019 Facal et al.’s research explored the effect of cognitive reserve (CR) in transforming from mild cognitive impairment (MCI) to dementia using both traditional and ML-based approaches. Using Petersen criteria for diagnosis, 169 participants who completed the longitudinal study were divided into three MCI subgroups, and a healthy control group. The authors utilized nine ML categorization algorithms to analyze collected data for prediction concerning ‘converter’ and ‘non converter’ participants from MCI to dementia. The top-performing ML models were i) the gradient boosting classifier with accuracy of 0.93, F1 of 0.86, and Cohen κ of 0.82, and ii) the RF classifier with an accuracy of 0.92, F1 of 0.79, and Cohen κ of 0.71. The authors, using ML techniques, demonstrated the protective role of CR as an arbitrator of conversion to dementia. Furthermore displaying that the participants with a) extra years of education and b) more outstanding vocabulary scores lived longer, deprived of developing dementia.38Zilcha-Mano et al., in 2018, used ML algorithms to identify predictors for antidepressant medication vs. placebo results in drug trials. 174 participants, with unipolar depression of age 75 and above, were randomly allocated to a pill (citalopram) or placebo. The authors used ML with ‘recursive partitioning’ algorithm to categorize the most robust arbitrators of placebo vs. medication response. The highest signal finding between medication and placebo in support of drugs was for patients with a lower education level (less than equal to 12 years) who experienced a longer duration of depression since their first incident. On the other hand, for individuals with higher education (more than 12 years), the placebo almost outpaced medication. Despite efforts to categorize characteristics associated with medication–placebo differences in antidepressant trials, few reliable findings have emerged to influence participant selection in drug development settings and differential therapeutics in clinical practice. Limitations in the methodologies used, mainly searching for a single moderator while treating all other variables as noise, may partially explain the failure to generate consistent results. The present study tested whether interactions between pretreatment patient characteristics, rather than a single-variable solution, may better predict who is most likely to benefit from placebo versus medication. The authors, for older patients with unipolar depression, recommended considering individuals’ education level and length of their depression in drug trials and also in clinical settings.39 - Challenges and opportunities for AI in psychiatry
AI by itself could not replace human empathy. Therefore, collaborations between ML and psychiatrists can be effective in diagnosis and treatment. AI-based technology might enhance psychiatrist’s efficiency and improve patient care, while reducing treatment costs. However, AI-based diagnosis in psychiatry is still not generally used in clinical practices as there are many legal, privacy, and ethical matters that impede its acceptance. - Conclusion
AI has the power to amplify clinical productivity due to its propensity to handle a vast amount of data suitable for automation. There exists a significant overlap in symptoms between mental disorders. AI is not going to substitute psychiatrists; instead it can provide psychiatrists with insights that can streamline treatment. AI with the potential to improve the accuracy of diagnosing different mood disorders and can assist psychiatrists in providing proper illness detection and subsequent treatment. - References
1. Richter T., Fishbain B., Markus, A., et al. “Using machine learning-based analysis for behavioral differentiation between anxiety and depression.” Sci Rep 2020;10:16381. https://doi.org/10.1038/s41598-020-72289-9.
2. Li X., Zhang X., Zhu J., et al. “Depression recognition using machine learning methods with different feature generation strategies.” Artificial Intelligence in Medicine 2019;99:101696. ISSN 0933-3657.
https://doi.org/10.1016/j.artmed.2019.07.004.
3. Dinga R., Marquand A., Veltman, D., et al. “Predicting the naturalistic course of depression from a wide range of clinical, psychological, and biological data: a machine learning approach.” Transl Psychiatry 2018;8:241. https://doi.org/10.1038/s41398-018-0289-1
4. Chekroud A., Zotti R., Shehzad Z., et al. “Cross-trial prediction of treatment outcome in depression: a machine learning approach.” The Lancet Psychiatry, 2016;3(3):243-250. ISSN 2215-0366. https://doi.org/10.1016/S2215-0366(15)00471-X.
5. Patel M., Andreescu C., Price J., et al. “Machine learning approaches for integrating clinical and imaging features in late-life depression classification and response prediction.” Int J Geriatr Psychiatry 2015;30:1056– 1067. doi: 10.1002/gps.4262.
6. Hosseinifard B., Moradi M., Rostami R. “Classifying depression patients and normal subjects using machine learning techniques and nonlinear features from EEG signal.” Computer Methods and Programs in Biomedicine, 2013;109(3):339-345. ISSN 0169-2607. https://doi.org/10.1016/j.cmpb.2012.10.008.
7. Tomasik J., Han S., Barton-Owen G., et al. “A machine learning algorithm to differentiate bipolar disorder from major depressive disorder using an online mental health questionnaire and blood biomarker data.” Transl Psychiatry 2021;11:41. https://doi.org/10.1038/s41398-020-01181-x.
8. Siqueira Rotenberg L., Borges-Júnior R., Lafer B., et al. “Exploring machine learning to predict depressive relapses of bipolar disorder patients.” Journal of Affective Disorders, 2021;295:681-687. ISSN 0165-0327.
https://doi.org/10.1016/j.jad.2021.08.127.
9. Fernandes B., Karmakar C., Tamouza R., et al. “Precision psychiatry with immunological and cognitive biomarkers: a multi-domain prediction for the diagnosis of bipolar disorder or schizophrenia using machine learning.” Transl Psychiatry 2020;10:162. https://doi.org/10.1038/s41398-020-0836-4.
10. Belizario G., Borges Junior R., Salvini R., et al. “Predominant polarity classification and associated clinical variables in bipolar disorder: A machine learning approach.” Journal of Affective Disorders, 2019;245:279-282. ISSN 0165-0327. https://doi.org/10.1016/j.jad.2018.11.051.
11. Perez Arribas I., Goodwin G., Geddes J., et al. “A signature-based machine learning model for distinguishing bipolar disorder and borderline personality disorder.” Transl Psychiatry 2018;8:274. https://doi.org/10.1038/s41398-018-0334-0
12. Schnack H., Nieuwenhuis M., van Haren N., et al. “Can structural MRI aid in clinical classification? A machine learning study in two independent samples of patients with schizophrenia, bipolar disorder and healthy subjects.” NeuroImage 2014;84:299-306. ISSN 1053-8119.
https://doi.org/10.1016/j.neuroimage.2013.08.053.
13. Hong S., Liu Y., Cao B., et al. “Identification of suicidality in adolescent major depressive disorder patients using sMRI: A machine learning approach.” Journal of Affective Disorders 2021;280(A):72-76. ISSN 0165-0327.
https://doi.org/10.1016/j.jad.2020.10.077.
14. Agne N., Tisott C., Ballester P., et al. “Predictors of suicide attempt in patients with obsessive-compulsive disorder: An exploratory study with machine learning analysis.” Psychological Medicine, 2020:1-11 doi:10.1017/S0033291720002329.
15. Carson N., Mullin B., Sanchez M., et al. “Identification of suicidal behavior among psychiatrically hospitalized adolescents using natural language processing and machine learning of electronic health records.” PLOS ONE 2019;14(2):e0211116. https://doi.org/10.1371/journal.pone.0211116.
16. Jihoon O., Kyongsik Y., Ji-Hyun H., et al. “Classification of Suicide Attempts through a Machine Learning Algorithm Based on Multiple Systemic Psychiatric Scales.” Frontiers in Psychiatry 2017;8:1-8.
ISSN=1664-0640. DOI=10.3389/fpsyt.2017.00192. https://www.frontiersin.org/article/10.3389/fpsyt.2017.00192.
17. Passos I., Mwangi B., Cao B., et al. “Identifying a clinical signature of suicidality among patients with mood disorders: A pilot study using a machine learning approach.” Journal of Affective Disorders 2016;193:109-116. ISSN 0165-0327. https://doi.org/10.1016/j.jad.2015.12.066.
18. Gao K., Chen D., Robison A., et al. “Proteome-Informed Machine Learning Studies of Cocaine Addiction.” The Journal of Physical Chemistry Letters 2021;12(45):11122-11134. DOI: 10.1021/acs.jpclett.1c03133.
19. Choi J., Jung H-T, Ferrell A., et al. “Machine Learning-Based Nicotine Addiction Prediction Models for Youth E-Cigarette and Waterpipe (Hookah) Users.” Journal of Clinical Medicine 2021;10(5):972. https://doi.org/10.3390/jcm10050972.
20. Wang Y., Qin Yun., Li Hui., et al. “Identifying Internet Addiction and Evaluating the Efficacy of Treatment Based on Functional Connectivity Density: A Machine Learning Study.” Frontiers in Neuroscience 2021;15. ISSN=1662-453X. DOI=10.3389/fnins.2021.665578. https://www.frontiersin.org/article/10.3389/fnins.2021.665578.
21. Symons M., Feeney G., Gallagher M., et al. “Machine learning vs addiction therapists: A pilot study predicting alcohol dependence treatment outcome from patient data in behavior therapy with adjunctive medication.”
Journal of Substance Abuse Treatment 2019;99:156-162. ISSN 0740-5472.
https://doi.org/10.1016/j.jsat.2019.01.020.
22. Hofmann L., Lau S., Kirchebner J. ” Advantages of Machine Learning in Forensic Psychiatric Research—Uncovering the Complexities of Aggressive Behavior in Schizophrenia..” Applied Sciences 2022;12(2):819. https://doi.org/10.3390/app12020819.
23. Watts D., Moulden H., Mamak M., et al.”Predicting offenses among individuals with psychiatric disorders – A machine learning approach.” Journal of Psychiatric Research 2021;138:146-154. ISSN 0022-3956.
https://doi.org/10.1016/j.jpsychires.2021.03.026.
24. Philipp G., Johannes K., Steffen L. “Identifying Direct Coercion in a High Risk Subgroup of Offender Patients With Schizophrenia via Machine Learning Algorithms.” Frontiers in Psychiatry 2020;11 ISSN=1664-0640. DOI=10.3389/fpsyt.2020.00415.
https://www.frontiersin.org/article/10.3389/fpsyt.2020.00415.
25. Randa C., Permanasari A. “Development of diagnosis expert system for personality disorders.” Conference: 2014 Makassar International Conference on Electrical Engineering and Informatics (MICEEI) 2014:180-183. DOI:10.1109/MICEEI.2014.7067335.
26. Berdahl C. “A neural network model of Borderline Personality Disorder.” Neural Networks 2010;23(2):177-188. ISSN 0893-6080. https://doi.org/10.1016/j.neunet.2009.10.007.
27. Hayat C., Limong S., Sagla N. “Architecture of Back Propagation Neural Network Model for Early Detection of Tendency to Type B Personality Disorders.” Khazanah Informatika : Jurnal Ilmu Komputer dan Informatika, 2019:115-123. ISSN 2477-698X. https://journals.ums.ac.id/index.php/khif/article/view/7923/5216.
28. Dobias M., Sugarman M., Mullarkey M., et al. “Predicting Mental Health Treatment Access Among Adolescents With Elevated Depressive Symptoms: Machine Learning Approaches.” Adm Policy Ment Health 2022;49:88–103. https://doi.org/10.1007/s10488-021-01146-2
29. Haque U., Kabir E., Khanam R. “Detection of child depression using machine learning methods.” PLoS ONE 2021;16(12):e0261131. https://doi.org/10.1371/journal.pone.0261131.
30. Price M., Albaugh M., Hahn S. et al. “Examination of the association between exposure to childhood maltreatment and brain structure in young adults: a machine learning analysis.” Neuropsychopharmacol. 2021;46:1888-1894. https://doi.org/10.1038/s41386-021-00987-7.
31. McGinnis R., McGinnis E., Hruschak J., et al. “Wearable sensors and machine learning diagnose anxiety and depression in young children.” 2018 IEEE EMBS International Conference on Biomedical & Health Informatics (BHI) 2018:410-413. doi: 10.1109/BHI.2018.8333455.
32. Saxe G., Ma S., Ren J., et al. “Machine learning methods to predict child posttraumatic stress: a proof of concept study.” BMC Psychiatry 2017;17: 223. https://doi.org/10.1186/s12888-017-1384-1.
33. Delavarian M., Towhidkhah F., Gharibzadeh S., et al. “Automatic classification of hyperactive children: Comparing multiple artificial intelligence approaches.” Neuroscience Letters 2011;3:190-193. ISSN 0304-3940. doi:10.1016/j.neulet.2011.03.012.
34. Anuradha J., Tisha T., Ramachandran V., et al. “Diagnosis of ADHD using SVM algorithm.” COMPUTE 2010- The 3rd Annual ACM Bangalore Conference. DOI:10.1145/1754288.1754317.
35. Ariyarathne G., De Silva S., Dayarathna S., et al. “ADHD Identification using Convolutional Neural Network with Seed-based Approach for fMRI Data.” ICSCA 2020: 2020 9th International Conference on Software and Computer Applications 2020:31-35. DOI:10.1145/3384544.3384552.
36. Yadgir S., Engstrom C., Jacobsohn G., et al. “Machine learning-assisted screening for cognitive impairment in the emergency department.” J Am Geriatr Soc. 2021;1-7. doi:10.1111/jgs.17491.
37. Hemrungrojn S., Tangwongchai S., Charoenboon T., et al. “Use of the Montreal Cognitive Assessment Thai Version to Discriminate Amnestic Mild Cognitive Impairment from Alzheimer’s Disease and Healthy Controls: Machine Learning Results.” Dement Geriatr Cogn Disord 2021;50:183-194. doi: 10.1159/000517822.
38. Facal D., Valladares-Rodriguez S., Lojo-Seoane C., et al. “Machine learning approaches to studying the role of cognitive reserve in conversion from mild cognitive impairment to dementia.” Int J Geriatr Psychiatry 2019;34:941-949. https://doi.org/10.1002/gps.5090.
39. Zilcha-Mano S., Roose S., Brown P., et al. “A Machine Learning Approach to Identifying Placebo Responders in Late-Life Depression Trials.” The American Journal of Geriatric Psychiatry 2018;26(6):669-677.
ISSN 1064-7481. https://doi.org/10.1016/j.jagp.2018.01.001.
- AI in depression

