ABSTRACT
Kulkarni, Rohan. M.S. Department of Microbiology and Immunology, Wright State University, 2016. Ebola: An Airborne Menace? A look in to Ebola’s Potential to Spread by Air
The Ebola outbreak in 2014 was clearly different in both size and scope than all the prior outbreaks. The outbreak initiated more human to human transmission of the virus than what had occurred in the prior few hundred years. As a RNA based virus, Ebola is sloppy at replicating and causes mutations as the virus may change between a transmission between the first two individuals than the next. The potential for mutations of the virus to allow it to become airborne is the central question of this report. Understanding different routes of Ebola virus transmission between humans is a critical step to count the virus transmission. I propose experiments and approaches of data collection in understanding airborne virus transmission that will enhance the understanding of the world’s scientific community.
LIST OF FIGURES (from Chapter 6)
1A. Ebola Virus
1B. Genome
1C. Gene Expression and Replication of Ebola
2. Predicted risk of districts becoming affected
3. Summary of Models used to characterize Spread
4. Ebola virus disease
5. Ebola outbreaks, historical and current
6. Viral dynamics during the 2014 outbreak
7. Patient time courses of iSNV frequencies and viral copy number
8. Ebola Virus Cell Entry and Replication
9. Ebola Airborne Spread and Droplet Spread
10. Which vaccines are being tested and where?
Chapter 1
I. INTRODUCTION
The CDC reported that 2014 has been the first Ebola epidemic the world had ever seen. In 2014 Marcelo et al model predicted that about 3,362 subpopulations in 220 countries were going to be negatively impacted in the year. The epidemic severely did affect the countries of Sierra Leone, Guinea, Liberia, and Nigeria. However, the probability of international spread is going to increase consistently. Thus the mode of Ebola transmission needs to be explored to both prevent and treat the disease it brings on. Aerial transmission can be through aerosol (as in the case of the flu), droplets, or indirect (such as fomites). The hypothesis explored in this report is that Ebola has the potential to be an airborne virus if it finds suitable conditions, which will be analyzed throughout the duration of this paper. More importantly, the hypothesis that Ebola virus can spread via the aerial mechanism in contrary to what the CDC has stated.
Chapter 2
II. BACKGROUND
According to the CDC (2015), the pathway of how the Ebola virus gains entry into humans at the onset in an outbreak is not known. Ebola’s natural reservoir has yet to be discovered, as well, but scientists believe that the first patient was most likely infected though a fruit bat or other primates such as mammals like humans, bats, monkeys, and apes (Leroy et al, 2005). Per CDC, the incubation period, which is the time interval from infection with the Ebola virus to onset of symptoms, is 2 to 21 days (Figure 4). The first symptoms seen in humans are the sudden onset of fever, fatigue, muscle pain, headache, and sore throat. This is followed by vomiting, diarrhea, rash, impaired kidney and liver function, and both internal and external bleeding.
The CDC’s model that predicted the number of cases in the years of 2014-2015 presents itself with a few limitations. It may not be suitable to extrapolate current activities in order to predict future cases. Rainisch et al (2014) believed that the model may be more accurate under a prediction of only the first three months after the 2014 outbreak. This study also presents with it another limitation stating that the number of beds that patients are using may be inaccurate due to the turnover of patients.
CURRENT SITUATION
Explaining the 49 cases in Guinea and analyzing the disease’s spreading capability, a study by Rainisch et al (2014) analyzed available data at the date published. The authors looked at those infected from the weeks ending March 29, 2014 until August 16, 2014. They classified affected districts in Guinea as prefectures, Sierra Leone as districts, and Liberia as counties. These locations had all told the World Health Organization that there was greater than or equal to one likely or definite case of the Ebola virus.
The authors developed four regression models in order to determine probabilities that districts in countries bordering the three mainly affected countries would become affected. They did this by analyzing available data from calculated probabilities that a certain district would become disturbed by Ebola’s effects over 3 succeeding week Periods. These Periods include weeks 34-36 or Period 1, weeks 37-39 or Period 2, and weeks 40-42 or Period 3. The authors picked a good fit of the model due to the fact that 87 percent (27 out of 31) districts were placed in the higher half or those classified as probable to become affected by the disease were actually affected (Rainisch et al 2014).
The top three ranked districts in each respective country are listed as follows: Bamako (Mali), Pikine (Senegal), and Abidjan (Cote D-Ivoire). The study found that there was a higher likelihood for larger population districts that were near affected districts with higher case counts to become affected by the disease. This can be seen in the data from both Figure 2 and Figure 3 (Rainisch et al 2014).
DIAGNOSIS AND TREATMENT
According to the WHO (2016), Ebola is hard to distinguish from other diseases like meningitis, malaria, or typhoid fever. Thus, in order to check that the symptoms present in an infected person are in fact from the Ebola virus the following methods can be used for validation of the disease: antigen-capture detection tests, electron microscopy, virus isolation by cell culture, reverse transcriptase polymerase chain reaction assay (RT-PCR), serum neutralization test, and antibody-capture enzyme-linked immunosorbent assay (ELISA).
There is no treatment for Ebola infection, but it has been found that rehydration with either intravenous or oral fluids can aid an individual’s survivability. A few possible vaccines are currently undergoing testing in order to see if they are safe, but unfortunately no vaccine is available for those infected. Thus, preventive measures cannot be used for treatment. Certain possible treatments that may or may have not worked in the past can include immune therapies, drug therapies, or blood products. Preventive measures to delimit the spread of the devastating virus include case management, excellent laboratory service, surveillance and contact tracing, quick nontoxic burials, and social mobilization (WHO, 2016).
SAFETY PRECAUTIONS
In order to control an Ebola disaster an individual can reduce the risk of wildlife to human transmission by not eating the raw meat of monkeys/apes or that of fruit bats. If contact with these animals is necessary individuals should use gloves and other safe clothing. Meat of any animal in an affected area should always be cooked properly before eaten. Those infected should immediately be separated from those that are healthy in order to stop the propagation of the virus. Education by having a healthy environment and keeping daily good hygiene are also important health initiatives the general population can use as protective habits. Thus, proper hygiene includes washing hands after taking care of the sick at home or seeing those that are sick at the hospital. It should be noted that regulating the health of contacts for 21 days should be recorded. Prevention by decreasing the risk of human-to-human transmission can happen by using gloves at home while dealing with the sick (WHO, 2014).
Those that are extremely at risk of obtaining the deadly virus include health care workers, as they are in constant contact with the infected. Obvious use of hygiene, including that of breathing non-contaminated air and washing hands regularly should be followed at all times. A health care worker who is within 1 meter of an infected patient should wear a medical mask and goggles or a face shield, sterile gloves, and a long sleeved gown. Protective equipment should be implemented in order to escape contact with infected materials. Infected materials include an infected patient’s body fluids and blood on clothing or blood on other surfaces. Lab workers are a demographic that is at high risk for the diseases, as well. Thus, only trained staff should handle Ebola samples taken from animals or humans when testing is done in suitable laboratories (WHO, 2014).
Chapter 3
III.EBOLA
VIRUS STRUCTURE
Ebola virus, shown in Figure 1 (viralzone.expasy.org), consists of seven proteins of GP, NP, VP35, VP30, VP24, VP40, and RNA-dependent RNA Polymerase ‘L.’ NP is used to provoke the host innate immune response while VP24 is used as another antagonizer of the host immune response, specifically preventing the expression of IFN-alpha/beta induced gene expression. GP is very important for four functions. Not only does GP counteract the host’s adaptive immune response, but it counteracts the host’s antiviral response as well. GP is a critical component of the Ebola virus because it stimulates the induction of pro-inflammatory cytokines, and it decreases the endothelial barrier function.
VIRUS INFECTING HUMANS
In the past cases of Ebola, primates have been shown to infect humans through either direct contact or consumption of the actual primates. The virus can spread from one individual to another individual through direct contact via broken mucous membranes (present in the nose, mouth, or eyes) and broken skin with objects such as needles and syringes that have been contaminated by the virus (see Figure 4, CDC). Other modes of transmission include blood or body fluids such as saliva, sweat, urine, feces, vomit, semen, or breast milk of a person who is sick with Ebola. The Ebola virus can remain in semen and vaginal fluids even after recovery of the virus, and scientists state that patients should abstain from sexual contact for at least three months after recovery. The CDC has stated that the disease is not spread by food, air, or water. Health care providers can become infected with Ebola if they are not wearing appropriate personal protective equipment, and therefore hospitals and clinics can pose as a potential hazard.
INFECTION AND LACK OF VACCINE/ANTIVIRAL THERAPY
According to Sullivan et al (2003), it is hard to control Ebola virus because it has a very fast progression during the actual infection process. Thus, it is very difficult to create any acquired immunity. This leads to no effective vaccine or antiviral therapy against the actual virus. Ebola has a very effective replication process. The replication is so rapid that a host’s immune defenses are devastated. Our bodies fight the infection by using the inflammatory and adaptive immune systems in order to combat infection at the same time. The critical cells that are attacked are both macrophages and monocytes. Other cells affected are mononuclear phagocytes, endothelial cells, and hepatocytes when determining if a person is infected by the Ebola virus.
The outbreaks that occurred during the year 1996 in Gabon demonstrated that there was not much discrepancy between survivors’ and non-survivors’ viral antigen load. However, the immune responses did show some differences meaning that surviving the disease needed either the innate or initial immune response to infection. Survivors showed a clearance of the viral antigen, more representative or significant IgM response, and constant T-cell cytokine responses. On the other hand, the antibodies pertaining to the virus were not found in fatal cases. Gamma interferon, on the contrary, was found to be present after the infection. Ras-related nuclear protein (Ran) levels related to T-cell cytokines showed that there was a failure to create any adaptive immunity days before a lifespan is ended. It has been shown that increased levels of IFN-alpha, IFN-gamma, IL-10, and tumor necrosis factor alpha are related with death from Ebola (Sullivan et al, 2003).
Using monoclonal antibodies derived from the bone marrow of recovered patients have some potential to neutralize the virus. It is easier to immunologically protect a mouse compared to a guinea pig, as guinea pigs have a need for larger antibody doses. Thus, from looking at this it can be determined that there is not any protective immunity due to antibodies solely. Also, cellular immunity is extremely important in clearing out the virus. However, these antibodies can be used in future therapy, as a hyper immune serum taken from the above mentioned vaccinated animals. More studies need to be performed in order to allow for the best quality of therapy to be both developed and implemented (Sullivan et al, 2003).
CELL ENTRY
A study done by Shimojima et al (2006) shows that both the Ebola virus and Marburg virus can use a Tyro3 receptor, which includes Dtk (also called Brt, Etk2, Rse, Sky, Tif, or Tyro3), Mer ((also called Nyk or Tyro12), and Axl (also called Ark, Tyro7, or Ufo), in order to enter a cell. In this study they took a look at the cDNA library from cells in order to find out that the virus uses such receptors. A majority of cells (besides lymphocytes) have at least a few receptors belonging to this family, and they found that macrophages are the key targets of this type of infection. Thus, the cells had similar tropism to filiovirus. The authors observed that just like a simian both Axl and Dtk of the human species heightened GP mediated infection and also that Mer did help in the infection process but not nearly as much as the effects that both Axl and Dtk had. Therefore, the authors assessed effects of only Dtk and Axl cells and not Mer cells.
Recently Sakurai et al (2015) suggested that this virus uses a calcium channel defined as a TPC2 or two-pore channel 2. TPC2 is needed in order to incorporate the virus’ genome into the host cell. The surface glycoprotein of Ebola binds to the host cell’s receptors, which contain many carbohydrate proteins. Ebola enters cell using the process of engulfment (see Figure 8, CDC), specifically micropinocytosis (defined as a form of endocytosis in which a large fluid-filled vesicle is pinched off from the cell membrane). Afterwards this vesicle is brought inside the cell. Ebola glycoproteins are eventually cleaved after they are adopted into a membrane-bound vesicle, and these processes occur in both a reducing and acidic environment. Fusion of the virus most likely takes place between the protein termed NPC1 or Niemann-Pick C1 and the endosome. This fusion process is what allows Ebola to release the virus’ genetic material into the cell.
It was thought that L-type calcium channels were needed for entry, but it was discovered that Ebola infection still occurred even when one out of five compounds that block these channels were used. The effective inhibitors block nicotininc acid adenine dinucleotide phosphate or NAADP- stimulated intracellular calcium channels or TPCs. Thus, it was found that cells lacking small interfering RNA, small-molecule inhibitors, and TPC2 are needed for entry. Sakurai et al (2015) study finds that TPC2 is particular to the glycoprotein of Ebola, which indicates a unique endosomal pathway. The authors state that it is not necessary for fusion due to the fact that late endosomes that show TPC2 and not NPC1 had a positive correlation with infection of the host cells. Thus, before fusion even takes place there is an interaction between NPC1 and the glycoprotein.
VIRUS LIKE PARTICLES (VLPs)
A study by Gire et al (2014) shows that Ebola virus-like particles (EBOV-VLPs) composed of the glycoprotein GP1,2 and the matrix protein VP40 use macropinocytosis and clathrin-mediated endocytosis to enter cells. EBOV-VLPs applied to host cells induced actin-driven ruffling and enhanced FITC-dextran uptake, which indicated macropinocytosis as the main entry mechanism. This was further supported by inhibition of entry through inhibitors of actin polymerization (latrunculin A), Na+/H+-exchanger (EIPA), and PI3-kinase (wortmannin). In particular, the uptake was significantly reduced by the inhibition of the Na+/H+-exchanger activity, which is known to be critical for macropinocytosis. The finding that latrunculin A had a weaker effect on particle uptake might be due to two phenomena. First, depolymerization of actin filaments results in cell rounding and cell detachment. In order to avoid those processes, latrunculin A had to be used at lower concentrations that only partially block actin polymerization and thus may still allow limited entry of particles. Second, a smaller number of particles might enter the cells by a different mechanism such as clathrin-mediated uptake as identified here, a phenomenon that might be related to differences in particle size. Particle heterogeneity has been shown for both infectious EBOV and noninfectious EBOV-VLPs. Two modes of clathrin coat formation have been described: the classical small clathrin-coated pits, which form rapidly and mediate fast uptake, and the larger coated plaques, which are longer-lived structures depending on actin dynamics and differing in uptake velocity and mechanisms.
Figure 6A shows 12 samples of the first outbreak of Ebola that occurred in patients from Sierra Leone. These individuals that had attended the funeral of an EVD from Guinea form two different clusters. Figure 6C shows that a single iSNV that is in common with twelve patients is later on seen as fixed within another 38 patients, making it the majority allele in the population. Figures 6A, and 6D show a third Sierra Leone cluster due to the fact that there has be a continuous propagation at halfway frequency. According to figure 6H the speed of nonsynonymous mutations shows that if this disease progression continues then the viral epidemic could evolve, and allow for viral adaptation to take place. According to supplemental figure S4 it was found that there were a total of 395 mutations with 50 of these classified as fixed nonsynonymous changes with eight at positions with high-levels of conservation among all the Ebola strains. Thus, this can open up further investigative studies in the near future (Gire et al, 2014).
VIRUS MUTATIONS LIKELY?
As per Evolution.Berkeley.Edu (2014), Ebola is a highly replicative virus with a high mutation rate, which provides more evidence that Ebola could transform into an airborne transmitted virus. A mutation is a very typical process that happens whenever an organism reproduces. Most of the mutations are completely random, and so it should be noted that mutations do not always generate bad or good effects as it depends on the mutation. Thus, the Ebola virus eventually incorporates the new mutations into the genomes every time reproduction of the virus takes place. Natural selection is how these mutations are passed down through generations, and then eventually spread through a population. Thus, the authors state that if Ebola were to incorporate the right mutations into its genome then the mutations would allow for transmission of Ebola through air. This lineage of transmission is advantageous because Ebola can spread by infecting hosts faster than non-airborne transmission.
The study states that Ebola has already had many mutations. Ebola is a RNA virus, and when RNA is copied there is a higher error rate compared to when DNA is copied. Thus, RNA viruses like Ebola have high mutations in comparison with DNA based viruses like chickenpox and smallpox. Ebola has the potential to evolve rapidly, as it has both a rapid rate of replication and a large mutation rate. Genetic variation is therefore created due to this high mutation rate. Unfortunately for the human species, if Ebola undergoes processes like ‘genetic drift’ and ‘natural selection’ it can then cause devastating evolutionary effects (Evolution.Berkeley.edu, 2014).
The 2014 outbreak has shown that Ebola has progressed quicker than it has in past outbreaks. The evolution of Ebola has gone at such a rapid rate maybe because it spreads through humans. This is because Ebola spread within wild animals such as between bats, and during this time random mutations that allowed bats to have a more advantageous living condition that could allow for the mutation to be genetically favored and eventually spread. This is known as adaptation, and thus the virus becomes very adapted to its host. When this adaptation takes place the evolution would slow down in turn. However, now that the environment of the Ebola virus has changed (bat to human), natural selection most likely favors mutations that allow the virus to propagate and survive in its host (Evolution.Berkeley.edu, 2014).
Carroll et al (2013) state that HIV came from chimpanzees and eventually spread to humans, while SARS came from bats and eventually spread to humans. Ebola is similar to SARS in this case. However, the authors state that it is rare to see a virus change its mode of transmission. They take a look at the case of HIV, and show that it has been attacking humans for over a century, and the virus has always been transmitted through body fluids when it comes to human infectivity. The filovirus occurred 10,000 years ago, and so it may stick as a virus that only has transmission through body fluids. Thus, it may be unlikely but the authors are saying that natural selection, genetic drift, and mutations could allow the virus to become airborne. Thus, we should be concerned about its evolution. This is because there have been multiple mutations located in the part of its genome, where diagnostic tests are implemented to identify the disease. Too many mutations could negatively impact remedies for curing the disease and developing medical vaccines. Various mutations can also make it so our standard tests become inaccurate, which in turn can make it hard to diagnose this virus.
POSSIBLE TREATMENT
Per Gupta et al (2001) study Tetrandrine, which is a drug that blocks TPC2’s channel activity, allowed mice that were infected by Ebola to survive, which proves TPC2’s critical role in infectivity. However, tetrandrine is not a probable treatment in humans, as it is originally a traditional Chinese medicine present in the plant Stephania tetrandra. Also, the doses given to the mice were way over the safe administration for humans. As of now, there are over 60 compounds that have been proposed to be useful against Ebola virus, but most of these compounds do not have a well-defined mechanism of action, whereas there is some such understanding for tetrandrine. A few of the compounds have advanced to clinical trials for Ebola (e.g., brincidofovir and favipiravir) largely in the absence of convincing preclinical data.
UPDATE FROM WHO (OCTOBER 2015)
Figures 10 through 13 compile a survey of drug trials for the virus.
Figure 10 shows that throughout the world many drug companies are conducting clinical vaccines trials (Phases I through III) for Ebola.
Figure 11 demonstrates which other treatments, therapies, or devices are available or being evaluated. Particularly transfusion of convalescent whole blood and plasma has been prioritized for use as an investigational therapy and are in Phase II and III of clinical trials.
In Figure 12 various pre-existing medicines that were considered for re-purposing to treat Ebola, several are either being tested (and are in Phase I through III of clinical trials) or considered for testing in patients with EVD or have already been used in patients with EVD.
Figure 13 describes how Ebola virus disease (EVD) is diagnosed. Because the symptoms for EVD are similar to the onset of many diseases (including influenza and malaria) the best alternative to diagnose if someone with suggestive symptoms is infected is to take a body sample, such as blood, and send it to a laboratory with proper equipment to handle potential Ebola specimens.
ANIMAL MODELS
In terms of vaccine development, necessary animal models include both Non-Human (NH) primates and guinea pigs, as the Ebola virus progression and pathogenesis is similar to that of the human disease. A mouse model was also created, but is considered more dissimilar to the human model, as it needs a serially passaged attenuated virus. NH primate infection is labeled the most predictive and necessary animal for vaccine development. Guinea pigs are similar to humans, as time course and symptoms of Ebola are the same. Recently, live attenuated viruses and recombinant proteins have been effective in a variety of vaccines. However, gene-based vaccines seem more likely to be made since they are safe. This type of approach has one important example of naked plasmid DNA, as this type of DNA has been proven effective in animal models. In these models the DNA directs the creation of immunogens inside the host cells. This inserted plasmid DNA created for the guinea pig model was the primary Ebola virus that worked. NP is what showed a humoral response, and was not as effective. On the other hand, both GP and sGP showed high proliferation of T-cells and cytotoxic responses. Humoral response was also increased, and this type of protection was important as only GP or sGP provided long-lasting protection in animals infected within 1 month of the last immunization. Thus, the importance of the effectiveness of NP still remains uncertain (Sullivan et al, 2003).
Limitations with Sullivan et al (2003) study are the fact that the vaccines do not seem to be as effective in human or primates compared to the effectiveness of the vaccines for the rodent models. DNA immunization pertaining to priming-boosting immunization, as boosting with poxvirus vectors containing the genes for pathogen proteins showed enhanced immune responses specifically in animal studies, as 30 fold or greater is higher in antibody titer related to the booster. An accelerated vaccination has been shown to be effective in nonhuman primates after one immunization, and so if this worked in humans it would work in containing small outbreaks by implementing this vaccination.
Sullivan et al (2003) state that it has been very hard to acquire Ebola samples because individuals with the disease live in remote areas. Therefore, the exact pathways for how the Ebola virus spreads into its’ host has not been fully mapped out. However, studying isolated cDNAs of the virus under suitable conditions has led to understanding the mechanism as to what happens to the cell during the virus’ infectivity. The virus is very similar to the Marburg Virus, as they are both part of the same Filovirus family. This family of virus is characteristic of having negative-sense RNA. Ebola is 19kb long with seven open reading frames. These frames include nucleoprotein, virion envelope protein, matrix proteins (VP24 and VP40), and nonstructural proteins (VP30 and VP35). The virus also contains viral polymerase. The open reading frame of this particular virus produces approximately 70 kDa or sGP and an approximately full length 170 kDa or GP protein. This protein both eventually attach onto the viral membrane. The envelope glycoprotein or GP binds mainly to endothelial cells, while sGP does not. GP is a trimeric complex, while sGP forms a dimeric protein. It was found that GP likes to bind to the endothelium using pseudo typing experiments in order to measure cell numbers, virus titers, and confluence, as well as experiments showing direct binding as in the case of fluorescence activated cell sorter analysis. Scientists have not discovered the receptors needed in order for the virus to initiate cell binding. It has also been found out that folate-related receptor may assist in the infection process. DC-SIGN may be able to allow the envelope glycoprotein or GP to bind to cells using viral carbohydrate determinants. On the other hand, sGP is used in neutrophil cell binding using CD16b, which is a specific neutrophil Fcgamma receptor III. According to Sullivan et al (2003) study immunoglobulin G was necessary to demonstrate binding.
Lee et al (2009) created a crystal structure depicting the trimeric ZEBOV GP that is in complex with KZ52, which happens to be an antibody discovered in a human survivor. The authors cut out the mucin-like domain and trans membrane domains, two N-linked glycosylation sites, at positions 40 and 22. Also, the GP was complexed with KZ52, which recognizes GP1/GP2 containing epitope. Two subunits of GP protein were found: Zebov GP1 and Zebov GP2. The GP1 subunit is necessary for the attachment to cells and contains many receptor-binding regions and a glycolated mucin-like domain. GP1 is composed of a base, head, and glycan cap. On the other hand, the GP2 subunit is needed in order to fuse the host and viral cell membranes together. This subunit consists of a hydrophobic internal fusion loop, CX6CC disulfide bond motif, two heptad repeats, membrane-proximal external region, and a trans membrane anchor. GP1 serves as a clamp on GP2, as four non-continuous stretches of GP1 fold together in order to create a hydrophobic beta sheet surface or GP1 base subdomain. This subdomain clamps on one of the heptad repeats of the GP2 and prevents it from going onto the fusogenic state too early. It was discovered using both structural and mutational studies since they found that three distinct putative receptor-binding sites are present in the trimer and are located inside the bowl of the chalice.
Weissenhorn et al (1998) found that viral and host cell membrane fusion is mediated by GP2, analogous to other class I viral fusion proteins, such as influenza virus HA2 and HIV-1 gp41. Removing the constraints of GP1 allows the GP2 HR1 to form a single 44-residue helix and place the loop on top of GP for insertion into the host membrane, which is termed a prehairpin intermediate. Formation of the low energy six-helix bundle enters the internal fusion loops and trans membrane domains, which creates the fusion pore and finally merges of the host and viral membranes.
Chapter 4
IV. EBOLA, AN AIRBORNE MENANCE?
According to the CDC (2014) Ebola is not considered an airborne virus, although they say that Ebola is spread through aerosol droplets. However, my hypothesis, contrary to the CDC’s views, states that Ebola potentially is an airborne virus or at least has the ability to become an airborne virus through mutation. The CDC states that you can get this particular disease from body fluids such as blood, diarrhea, vomit, semen, breast milk, and urine. Cuts through the skin are another way of the disease-spread process. Figure 9 (by CDC) explains the difference between the two ways of virus transmission. Droplet spread is said to happen when an infected person can spread droplets that are large in size by spraying a non-infected person’s nose, mouth, or eyes. This would most likely occur due to a conversation with an infected person, and the infected person accidentally spitting saliva/mucus on another person. Droplet spread can also occur through soiled bathroom handrails or other environmental uncleanliness. The CDC states that airborne spread, on the other hand, floats through the air after coughing, sneezing, or talking. They even state that in airborne transmission the germs can be inhaled after the infected person leaves the area.
This pamphlet has many errors in it and it is puzzlingly why it was printed. This said because the authors contradict themselves when contrasting airborne spread (diseases like TB and chicken pox) and droplet spread (disease such as plague) because they state “droplet spread happens when fluids in large droplets from a sick person splash the eyes, nose, or mouth of another person”. Then they say that airborne spread occurs “after a person talks, coughs, or sneezes” (CDC, 2014).
Osterholm et al (2015) say that Ebola does have a potential to be spread airborne through respiration. The authors state that both airborne transmission and droplet transmission can be classified under the same category termed aerosol transmission, thus agreeing with my hypothesis stating that the two should not be contrasted in the first place. They state that strong secretions from body fluids like diarrhea or vomit can create aerosols that enter the respiratory tract. This type of transmission occurs through infecting another person by entering a non-infected person’s trachea, lungs, or nasal passages. These aerosols then enter the airspace, and the authors believe that when these germs are in the airspace this transmission is a droplet or an airborne type.
Osterholm et al (2015) study states that the aerosol particles can range from 5-100 micrometer in diameter and infect through skin, mucous membranes, and other surfaces. Inhalation can occur from taking in the small airborne particles even at a distance from the said surface. They disagree with the CDC because large particles can be inhaled from a person when these particles have been suspended in air or on an infected surface nearby. The authors state that epidemiology and the way of transmission of this disease need to be looked into further.
According to Judson et al (2015), Ebola can spread via the air according to experiments in NHPs. Experiments in the past looking at the virus’ transmission showed that Ebola could be aerosolized to small droplet or droplet nuclei size, which in turn could lead to the disease in rhesus macaques after inhalation of at least 400 pfu. Even more alarming are the recent experiments that show that inhaling less than ten pfu of EBOV is enough to cause the disease. It should be noted that the Ebola virus used in this experiment was ‘aerosolized mechanically,’ and it was not brought up that whether Ebola could become ‘aerosolized naturally.’ The experiments were performed in a 24 degrees Celsius and less than 40% relative humidity, which represent the American climate and not the African climate where the outbreaks have taken place.
More concern about Ebola being an airborne virus is the fact the Reston virus, which is in the same genus as the Ebola virus, indirectly infected naïve NHPs in distant cages. The airborne mechanism thus needs to be examined more critically, as the authors state that cleansing the cages of infect animals may have contributed to the formation of aerosols containing the Ebola virus (Judson et al, 2015).
Kilianski et al (2015) find that the science supporting or refuting the aerosol transmission of EBOV remains unclear, the word “aerosol” carries significant weight in public discourse and therefore the media and scientific community should be cautious in their interpretation.
PROPOSED SERIES OF EXPERIMENTS TO ASSESS IF EBOLA TRANSMISSION CAN HAPPEN BY AN AIRBORNE MECHANISM
Per CDC (2014), we know that Ebola can be contracted through direct contact with bodily fluids. The current Ebola virus’s tremendous evolution is unique since there has been more human-to-human transmission in the past outbreak in 2014 than had occurred in the last few hundred years (WHO, 2014). The key reason for this is that, unlike DNA based viruses, RNA based viruses like Ebola are sloppy in replicating (Evolution.Berkeley.edu, 2014). This creates a situation where the virus entering one person may be genetically different from the virus infecting the next individual. To answer a question that an Ebola virus could mutate to become transmissible through the air a series of experiments is therefore devised.
Darling et al (2004) exposed non-human primates to aerosolized Ebola virus from pigs became infected; however, airborne transmission was not been demonstrated between NH primates in this study. In the work performed by Kobinger et al (2011) and Marsh et al (2011), viral shedding was observed in nasopharyngeal secretions and rectal swabs of pigs following experimental inoculation.
Osterholm et al (2015) suggest that at least some degree of Ebola virus transmission currently occurs via infectious aerosols generated from the gastrointestinal tract, the respiratory tract, or medical procedures. However, this has been difficult to definitively demonstrate or rule out, since those exposed to infectious aerosols also are most likely to be in close proximity to and in direct contact with an infected case.
Per CDC (1989), Ebola Reston virus among monkeys was transmitted through breathing. In 1989, macaques monkeys imported from the Philippines died at Hazelton Research Products’ primate quarantine unit in Reston. These animals were kept in this facility and later sold for lab testing. The company’s officials contacted the U.S. Army concerned that they may be dealing with an outbreak of hemorrhagic fever among the monkeys.
Initial testing revealed something much worse that Ebola (the Zaire strain), which had a 90 percent fatality rate in humans. Four workers at the facility tested positive for exposure to the virus. Surprisingly, the workers never got sick!
Jaax et al (1995) reported transmission of Zaire strain Ebola virus to two out of three control rhesus monkeys (Macaca mulatta) without direct contact with experimentally inoculated monkeys kept in the same room. The two control monkeys died from Ebola virus infections 10 to 11 days after the last experimentally inoculated monkey had died. The most likely route of infection of the control monkeys was aerosol, oral or conjunctival exposure to virus-laden droplets secreted or excreted from the experimentally inoculated monkeys.
Johnson et al (1995) established a potential of aerogenic infection by Ebola virus by using a head-only exposure aerosol system. In this study, virus-containing droplets of 0.8-1.2 microns were mechanically generated and administered into the respiratory tract of rhesus monkeys via inhalation. Inhalation of viral doses (as low as 400 plaque-forming units or Pfus of virus) caused a rapidly fatal disease in 4-5 days. This illness was clinically identical to that reported of parenteral virus inoculation, except for the occurrence of subcutaneous and venipuncture site bleeding and serosanguinous nasal discharge.
Weingartl et al (2012) showed Zaire-Ebola Virus (ZEBOV) transmission from pigs to cynomolgus macaques monkeys without direct contact. Interestingly, this type of transmission between macaques in similar housing conditions was never observed. In this study, piglets inoculated oro-nasally with ZEBOV were transferred to the room housing macaques in an open inaccessible cage system. All macaques became infected with virus being detected in oro-nasal swabs of piglets, and in blood, swabs, and tissues of macaques. This is the first experimental interspecies virus transmission study, with the macaques used as a human surrogate.
Judson et al (2015) demonstrated that (Figure 15 contact with isolated bodily fluids (blood, stool, semen, saliva, and breast milk) from EBOV infected individuals creates a high risk of virus transmission. These fluids can also be formed into droplets which travel in the air (range not known – possibly 1 m) and potentially can infect others. The virus can be detected in dried blood and persists on surfaces creating a possibility of fomite transmission of the virus. Airborne transmission via small aerosol droplets is unlikely according to this study. The study, for each of the possible transmissions mechanisms, there are many unknowns about how the virus transmits from an infected person. For aerosol method of transmission, unknowns are ability of the virus becoming airborne through respiratory tract in humans or animals, airborne stability of the virus in tropical climates, and if Aerosol Generating Procedures (AGPs) can produce virus aerosols that cause transmission. The likely unknown for fomite transmission is virus’s stability in tropical climates and on surfaces. Unknowns for ‘droplet’ transmission are if the body fluids are formed into droplets by humans and also range of droplets containing the virus. For a direct contact method of transmission unknown is the amount of virus shed in the body fluids.
Airborne/aerosol transmission occurs when small droplets with EBOV evaporate and settle on surface, allowing infectious droplet nuclei (aerosol) to travel long distances (Judson et al, 2015). Infectious droplet nuclei are formed when small droplets evaporate before settling on surfaces during airborne or aerosol transmission. These droplet nuclei can travel long distances. Some scientists define aerosols as droplets that can form droplet nuclei. However, aerosols are defined as suspended small liquid or solid particles. Some researchers state that small droplets are smaller than 20 µm and that the size of droplet-nuclei are smaller than 5 µm.
The authors also claim that NHPs catching the disease was based on a ‘mechanically aerosolized’ and not ‘naturally aerosolized’ based virus transmission. The aerosolized based studies were conducted at 24C and < 40% relative humidity which is not representative of African environment. Also the study claims that pressure washing of animal cages may have set the virus airborne (droplets or aerosols) in the pigs to monkeys transmission of virus without contact. Also, biosafety 4 level labs (BSL-4) where typical EBOV transmission experiments are run have pressure driven airflow. Pressure driven flow might affect the path of the virus in the airflow.
Droplet/large droplet transmission occurs with a contact w/ infectious droplets that do not evaporate and do not travel long distances – marked as < 1 m per Judson et al (2015) study. This study claims lack of experimentation of EBOV droplets. In the Roels et al study (1995), five patients who became infected reported no contact with EBOV carrying patients but were in close proximity with them. This may be a case of EBOV droplet transmission.
Judson et al (2015) study proposes capturing ‘air samples’ for type of EBOV when the animal cages of infected animals are pressure washed. Per the study, fomite (surface that a pathogen is able to persist on) transmission can occur when person comes in contact w/ an infected surface. Very little is known about stability/sustainability of virus on surface and more studies need to be conducted to understand this type of EBOV transmission.
Transmission of EBOV by bodily fluids (semen, saliva, blood, and breast milk) is a confirmed mechanism (Bausch et al, 2007 and CDC, 2014) and RNA has been present in sweat, stool, tears, and on skin/vaginal/rectal swabs. However, analysis, the amount of virus secreted in these fluids is not known (Judson et al 2015).
There are thus many questions unanswered for each mechanism of EBOV transmission. Some of the important questions to consider are:
- At what temperature range and relative humidity range Ebola can be stable and sustain transmission by ‘droplet’ or ‘aerosol?’
- How does temperature, relative humidity, size of particle diameter containing EBOV affect stability/sustainability of the virus?
- Can experiments be conducted with one type of transmission and not the other (by aerosol only and not by droplet and by fomite)?
- What is the range (distance) of fomite transmission?
- Are aerosols and fomites generated by patients/humans? By animals?
To understand better all the mechanisms of transmission of Ebola virus, BSL-4 facility will allow us to help study many of the above questions. The study can be broken into three steps:
- Understand Temperature and Relative Humidity Effect on EBOV Transmission Mechanisms: Run a 2×2 factorial experiment with temperature (high: 40 C and low: 20C) and relative humidity (high: 70% and low: 30%) to capture virus stability on aerosol, droplet, and fomite transmission each. The BSL-4 room can be divided in circular coordinates to capture air samples for aerosol, droplet, and fomite and different radii. The source for EBOV will be mechanically aerosolized. Airflow rates in/out of the room will be controlled and kept at a low flow rate to avoid impeding virus transmission.
The temperature and humidity can be lowered further for subsequent studies to capture their effects on the virus stability/sustainability.
2) Understanding Particle Diameter Effect on EBOV Transmission Mechanisms: At critical temperature and relative humidity derived from the ‘step 1’ above, various particle size aerosols will be mechanically generated to understand their effects on aerosol, droplet, and fomite transmission of the virus.
Note that one can run a 3×3 factorial experiment with temperature, relative humidity, and particle size as factors (a very large experiment) by combining the above two steps.
3) NHP Experiment: Three types of NHP experiments will be run in parallel. One with NHPs exposed to pigs inoculated with EBOV (but without direct contact w/ NHPs) as a source where temperature and relative humidity will be varied based on the results of above two steps.
In the second study NHPs would be exposed to mechanically aerosolized EBOV where particle size will be varied and also distance of source to the cages will be varied to understand droplet versus aerosol transmission of the virus to NHPs. Room temperature and relative humidity will be varied based on the results of above two steps also.
If certain mutations were to occur, it would mean that just breathing would contract Ebola and spread quickly as the H1N1 influenza virus did (Tellier, 2009). In a third experimentation study, similar to highly pathogenic avian influenza virus study of Spekreijse et al (2013), the amount of virus shed by infected primates and its relation to deposition of virus in the environment and the rate of air-borne transmission (droplet or aerosol) will be quantified between groups of primates. Four replicate experiments in this study will be performed, each replicate with two groups of 14 primates housed in two separate rooms. In one group, primates will be inoculated with Ebola virus.
Per Franz et al (1997), viral hemorrhagic fevers have an ‘infectious dose’ (a quantity of a pathogen measured in number of organisms that is necessary to cause infection in a susceptible host) of 1 to 10 organisms by aerosol in non-human primates, which we will implement in our study. Ventilation will force the air from that room to the second (recipient) group through a tube. Deceased primates in the inoculated group will be replaced with new susceptible primates. Dust/air samples will be collected daily. Mouth swabs will be collected daily as well to determine virus shedding and virus spread to the recipient group.
Our testing and collection of data will include consideration of incubation period of two to 21 days for the virus (Darling et al, 2004 and Feigin, 2004) for all three experiments.
Chapter 5
V. SUMMARY AND CONCLUSIONS
In 2014 the world saw the first ever Ebola epidemic. As of August 2015, about 28,000 cases were reported worldwide in total with 11,300 deaths worldwide, the vast majority of them in Guinea, Liberia and Sierra Leone. The pathway of how the Ebola virus gains entry into humans at the onset is not known. Ebola’s natural reservoir has yet to be discovered, as well, but scientists most likely believe that the first patient is infected though a fruit bat or other primates. According to the WHO, diagnosis of Ebola is hard to distinguish from other diseases like meningitis malaria, or typhoid fever. There is no treatment for Ebola infection yet, but it has been found that rehydration with either intravenous or oral fluids can aid an individual’s survivability. A few possible vaccines are currently undergoing testing in order to see if they are safe for treatment of the human, but unfortunately no vaccine is available for those infected.
In Ebola infection of the human the Ebola virus can spread from one individual to another (through direct contact via broken mucous membranes in the nose, mouth, or eyes and broken skin) with objects such as needles and syringes that have been contaminated by the virus and infected fruit bats or primates. Other modes of transmission include blood or body fluids such as saliva, sweat, urine, feces, vomit, semen, or breast milk of a person who is sick with Ebola.
Per the CDC (2014) Ebola is not considered an airborne virus, although they say that Ebola is spread through aerosol droplets. However, my hypothesis goes against the CDC’s stance and says that Ebola potentially is an airborne virus or at least has the ability to become an airborne virus through mutation.
Per WHO (2014), Ebola outbreak in 2014 was clearly different in size and scope than all the prior outbreaks. There had been more human to human transmission of the virus than likely occurred in prior few hundred years. Being a RNA based virus, it is sloppy at replicating causing mutations as the virus may be different between a transmission between first two individuals than the next. Can certain mutations of the virus allow it to become airborne is the central question of this report. Per many scientists, science supporting or refuting the aerosol transmission of EBOV remains unclear. Therefore understanding different routes of Ebola virus transmission between humans is a critical step to count the virus transmission. In this paper I proposed a series of experiments to understand droplet/fomite/aerosol routes of virus transmission including approaches of data collection in understanding.
This series of experimentation would shed light on effects of temperature, relative humidity, size of virus particle diameter on airborne transmission. NH primate study, similar to highly pathogenic avian influenza, virus is further proposed in consideration with temperature/humidity/virus particle diameter to quantify the amount of virus shed by infected primates and its relation to deposition of virus in the environment and the rate of air-borne transmission between groups of primates.
Understanding of conditions required for an airborne (droplet/fomite/aerosol) spreading of Ebola virus thus would allow scientists to devise solutions against it.
Chapter 6
FIGURES
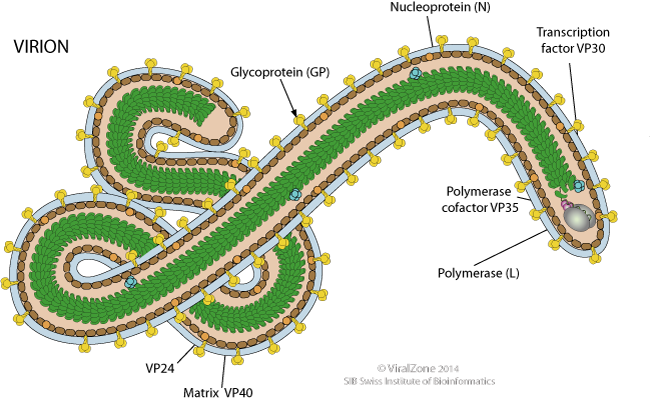
Filamentous 970 nm long for Ebolavirus. Diameter is about 80nm.
Figure 1A. Ebola Virus (Applied from ViralZone, 2014)
GENOME
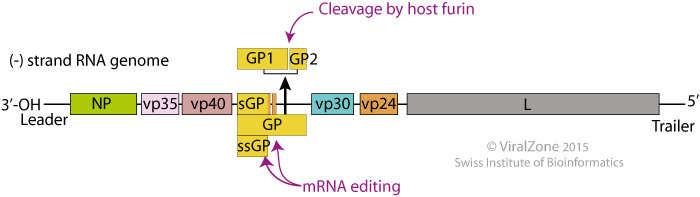
Negative-stranded RNA linear genome, 18-19 kb in size. Encodes for seven proteins.
Figure 1B. (Applied from Ebolavirus, Viralzone, 2014)
GENE EXPRESSION
The viral RNA dependent RNA polymerase binds the encapsidated genome at the leader region, then sequentially transcribes each genes by recognizing start and stop signals flanking viral genes. mRNAs are capped and polyadenylated by the L protein during synthesis.
The primary product of the unedited transcript of GP gene yields a smaller non-structural glycoprotein sGP which is efficiently secreted from infected cell. RNA editing allows expression of full-length GP.
REPLICATION
CYTOPLASMIC
- Attachment to host receptors through GP glycoprotein like DC-SIGN and DC-SIGNR
- Cellular receptor like HAVCR1 (TIM1) binds phosphatidyl serine on virion membrane and a signal is transduced into the cell that trigger the macropinocytosis program by apoptotic mimicry.
- The virion enters the cell by Macropinocytosis. In some culture cells, GP glycoprotein can be processed by host Cathepsin L and Cathepsin B into 19kDa GP1. But this processing is not happening in all cells or for all ebolavirus.
- GP1 interacts with host NPC1, in late macropinosome and promotes fusion of virus membrane with the vesicle membrane. The ribonucleocapsid is then released into the cytoplasm.
- Sequential transcription, viral mRNAs are capped and polyadenylated by polymerase stuttering in the cytoplasm.
- Replication presumably starts when enough nucleoprotein is present to encapsidate neo-synthetized antigenomes and genomes.
- The ribonucleocapsid interacts with the matrix protein, and buds via the host ESCRT complexes from the plasma membrane, releasing the virion .
Figure 1C. Gene Expression and Replication of Ebola (Applied from Ebolavirus, Viralzone, 2014)
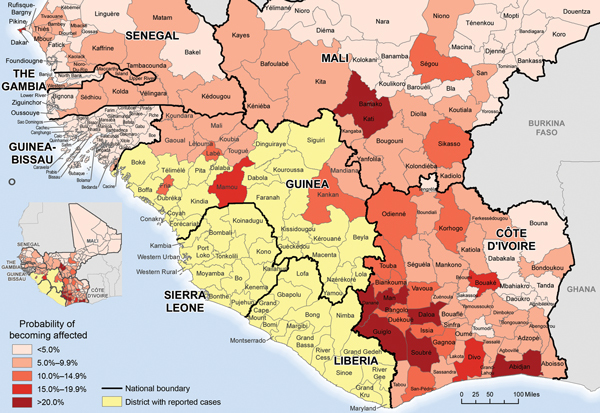
Predicted risk of districts becoming affected by Ebola virus infection (neighboring countries included) in 2014, based on data available through epidemiological week 42 (October 18, 2014).
Figure 2. (Applied from Rainisch et al, 2014)
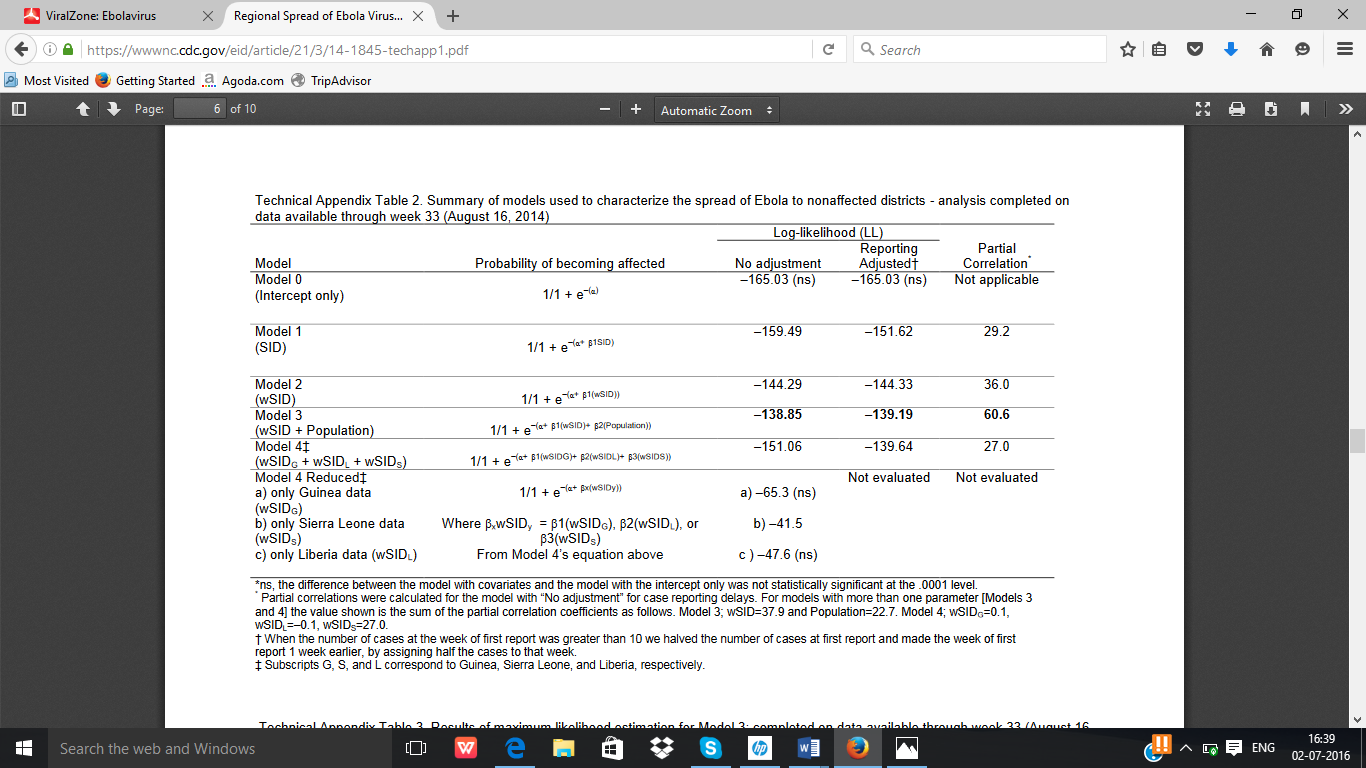
Summary of Models used to characterize Spread of Ebola to Non-Affected Districts
Figure 3. (Applied from Rainisch et al, 2014)
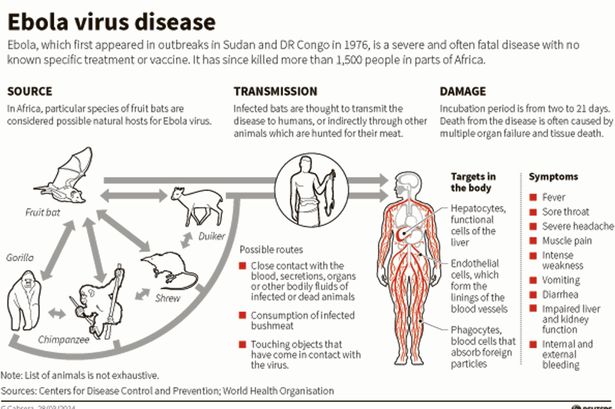
Figure 4. (Applied from CDC, 2014)
Ebola outbreaks, historical and current
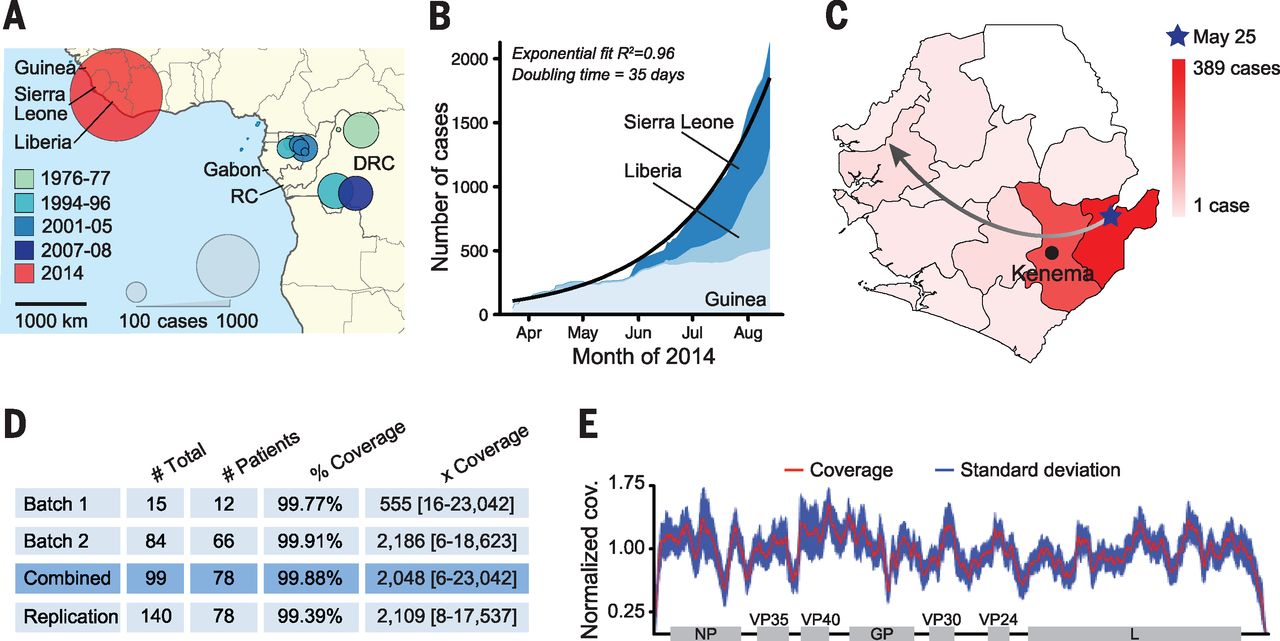
(A) Historical EVD outbreaks, colored by decade. Circle area represents total number of cases (RC = Republic of the Congo; DRC = Democratic Republic of Congo).
(B) 2014 outbreak growth (confirmed, probable, and suspected cases).
(C) Spread of EVD in Sierra Leone by district. The gradient denotes number of cases; the arrow depicts likely direction.
(D) EBOV samples from 78 patients were sequenced in two batches, totaling 99 viral genomes [replication = technical replicates]. Mean coverage and median depth of coverage with range are shown.
(E) Combined coverage (normalized to the sample average) across sequenced EBOV genomes.
Figure 5. (Applied from Gire et al, 2014)
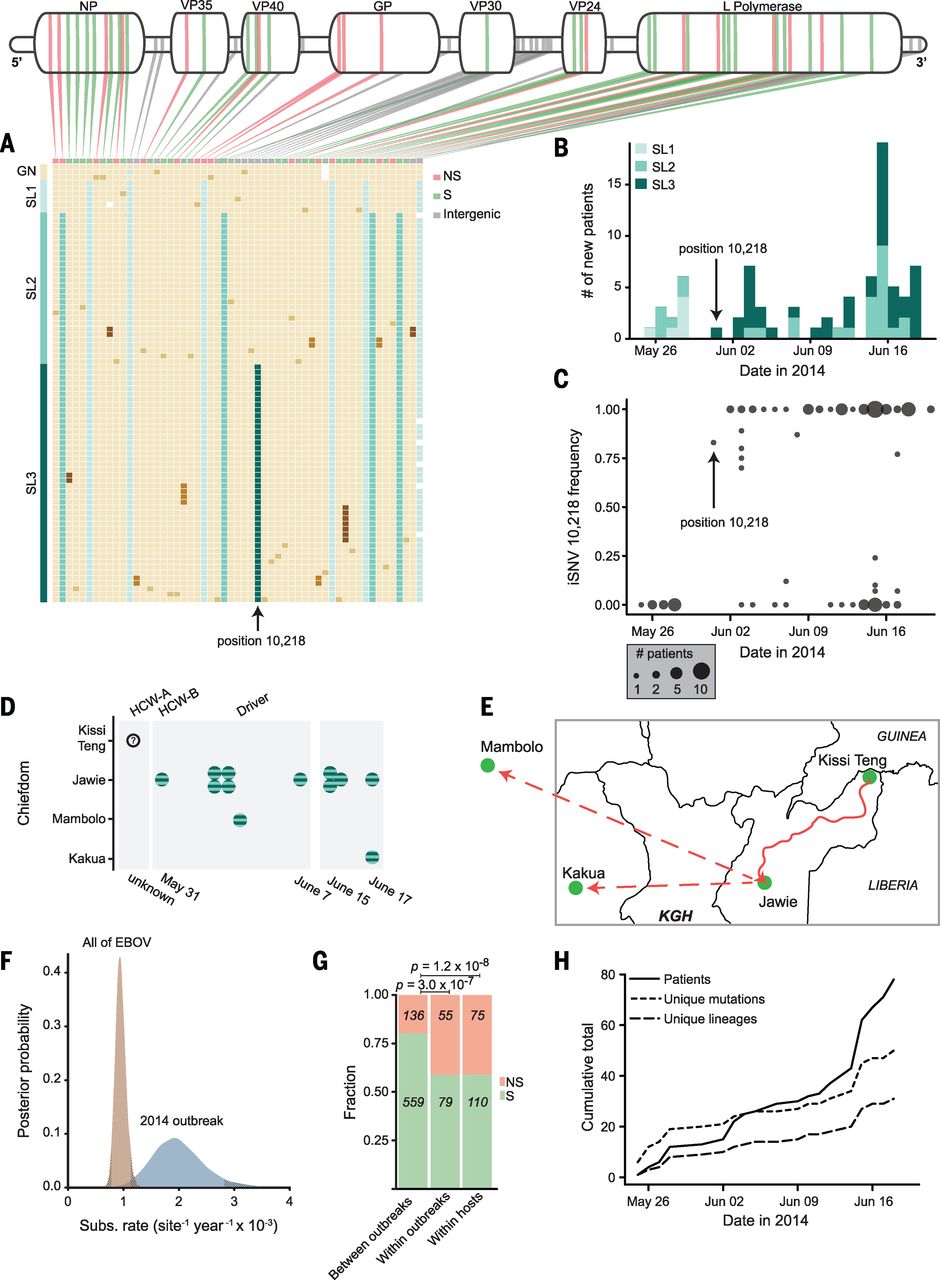
Figure 6. Viral Outbreak Dynamics(Applied from Gire et al, 2014)
Viral Dynamics Description during the 2014 outbreak
(A) Mutations, one patient sample per row; beige blocks indicate identity with the Kissidougou Guinean sequence (GenBank accession {“type”:”entrez-nucleotide”,”attrs”:{“text”:”KJ660346″,”term_id”:”674810549″,”term_text”:”KJ660346″}}KJ660346).The top row shows the type of mutation (green, synonymous; pink, nonsynonymous; gray, inter-genic), with genomic locations indicated above. Cluster assignments are shown at the left.
(B) Number of EVD-confirmed patients per day, colored by cluster. Arrow indicates the first appearance of the derived allele at position 10,218, distinguishing clusters 2 and 3.
(C) Intrahost frequency of SNP 10,218 in all 78 patients (absent in 28 patients, polymorphic in 12, fixed in 38).
(D and E) Twelve patients carrying iSNV 10,218 cluster geographically and temporally (HCW-A = unse-quenced health care worker; Driver drove HCW-A from Kissi Teng to Jawie, then continued alone to Mambolo; HCW-B treated HCW-A). KGH = location of Kenema Government Hospital.
(F) Substitution rates within the 2014 outbreak and between all EVD outbreaks.
(G) Proportion of nonsynonymous changes observed on different time scales (green, synonymous; pink, nonsynonymous).
(H) Acquisition of genetic variation over time. Fifty mutational events (short dashes) and 29 new viral lineages (long dashes) were observed (intrahost variants not included).
Figure 6. (Applied from Gire et al, 2014)
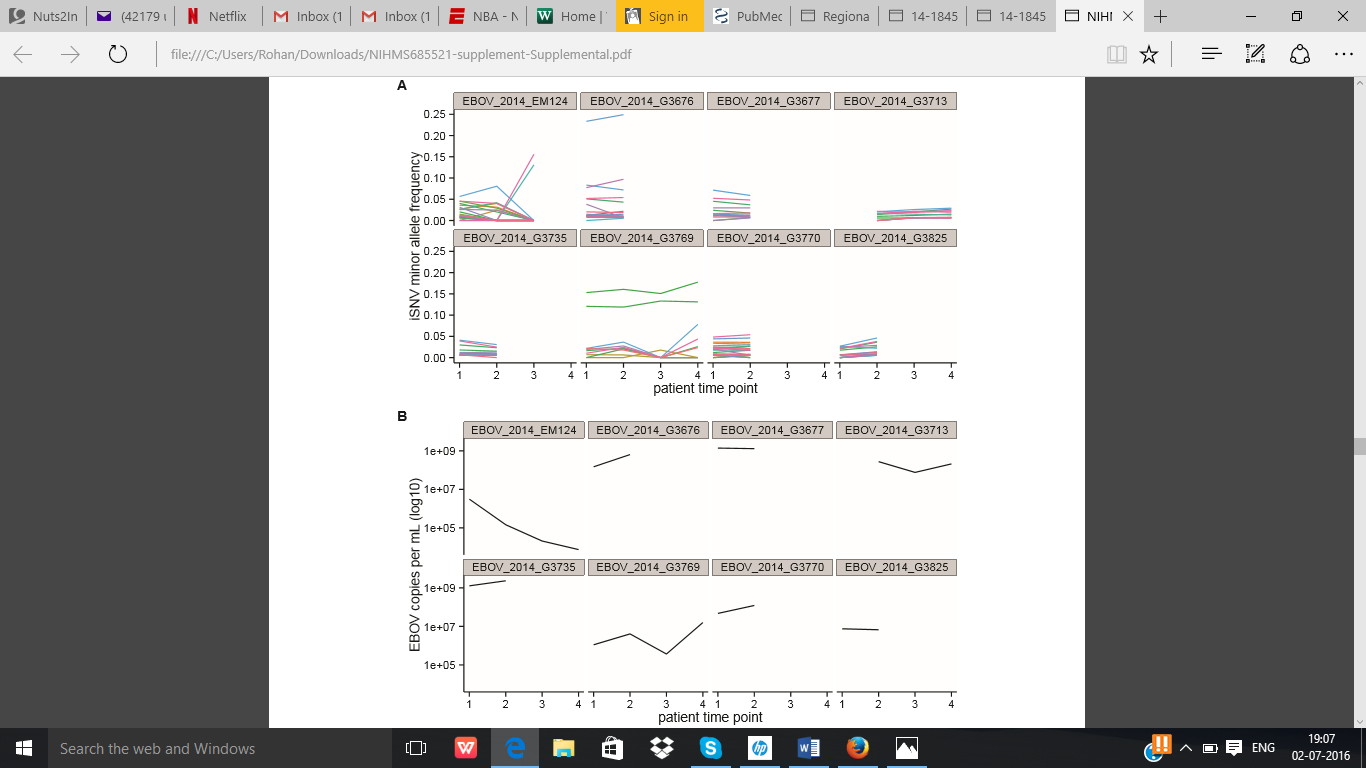
Patient time courses of iSNV frequencies and viral copy number. Figure 7. (Applied from Gire et al, Figure S4, 2014)
Description
(A) iSNV minor allele frequencies are generally stable across time for patients where multiple time points are available. Each color represents a different variant position in the genome. Both SNP and indel intrahost variants are shown here.
(B) Viral copy number (table S2) is shown at each time point. Note that the fourth time point of EM124 produced a consensus assembly, but did not provide sufficient read depth for the identification of iSNVs.
Figure 7 .(Applied from Gire et al, Figure S4, 2014)
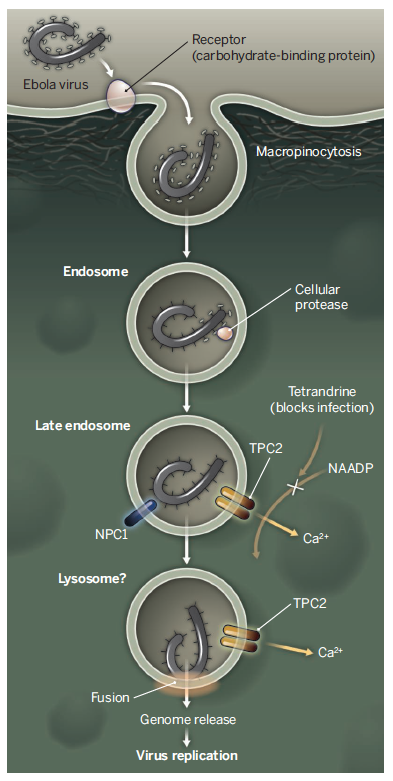
Ebola Virus Cell Entry and Replication
Figure 8. (Applied from CDC, 2014)
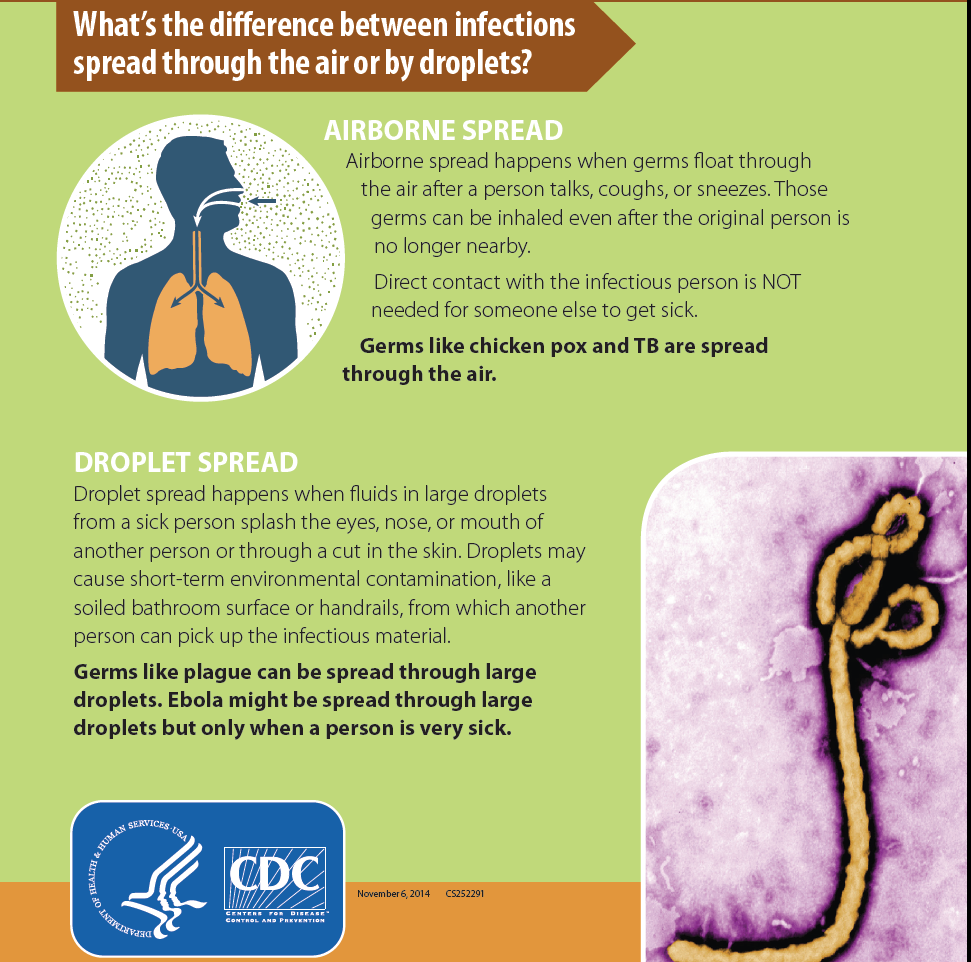
Ebola Airborne Spread and Droplet Spread
Figure 9. (Applied from CDC, 2014)
Figure 10. Which vaccines are being tested and where? (Applied from WHO, October 2015)
| Product / Company | Phase | Trial Location | Dates |
| ChAd3-ZEBOV
GlaxoSmithKline and PHAC |
Phase I | By VRC at NIH, USA | September 2014 |
| By Oxford University in the UK | |||
| By CVD in Mali | October 2014 | ||
| At the University of Lausanne, Lausanne, Switzerland | |||
| rVSV-ZEBOV
NewLink Genetics and Merck Vaccines USA |
Phase I | By WRAIR in the US | October 2014 |
| By NIAID in the US | |||
| By CTC North GmbH in Hamburg, Germany | November 2014 | ||
| At Albert Schweitzer Hospital in Lambarene, Gabon | |||
| At the University of Geneva, Geneva, Switzerland | |||
| At the IWK Health Center, Halifax, Canada | |||
| By KEMRI Wellcome Trust in Kilifi, Kenya | December 2014 | ||
| Ad26-EBOV and MVA-EBOV
Johnson & Johnson and Bavarian Nordic |
Phase I | By University of Oxford in the UK and NIAID, USA | January 2015 |
| TBD, Kenya | Second half of 2015 | ||
| TBD, Uganda | |||
| TBD, United Republic of Tanzania | |||
| Recombinant protein Ebola vaccine candidate
Novavax |
Phase I | Australia | February 2015 |
| ChAd3-ZEBOV
GlaxoSmithKline and PHAC |
Phase II | TBD, Cameroon | Second half of 2015 |
| TBD, Ghana | |||
| TBD, Mali | |||
| TBD, Nigeria | |||
| TBD, Senegal | |||
| VSV-EBOV
NewLink Genetics and Merck Vaccines USA |
Phase III | By WHO, Médecins Sans Frontiéres (MSF) and Government of Guinea in
Conakry, Guinea |
April 2015 –
Ring vaccination trial design. As of 17 July, 103 rings comprising approximately 4 000 volunteers have been vaccinated. |
| VSV-EBOV | Phase III | By Médecins Sans Frontiéres (MSF), WHO and Government of Guinea in Conakry, Guinea | March 2015 – A vaccine trial for front line workers only. As of 19 June, more than 800 volunteers have been vaccinated. The target number is 1 200. |
| ChAd3-ZEBOV
GlaxoSmithKline and PHAC and VSV-EBOV NewLink Genetics and Merck Vaccines USA |
Phase II/III | By US NIH and MOH Liberia in
Monrovia, Liberia |
March 2015 –
Randomized control trial design As of 30 April, Phase II enrollment of 1 500 volunteers in Liberia was completed. |
| VSV-EBOV
NewLink Genetics and Merck Vaccines USA |
Phase III | By US CDC and MOH Sierra Leone in
Freetown, Sierra Leone |
April 2015 –
Cluster based, non-blinded, individually randomized trial design. As of 18 June, approximately 6 000 frontline workers had been enrolled with half of them vaccinated. |
Pre-clinical trials
Pre-clinical trials are carried out in laboratories and animals and aim to: 1) determine whether a vaccine works as intended and 2) to identify any harmful effects.
Clinical trials
Phase I trials involve 20 to a few hundred healthy individuals and examine safety and immune response. They also identify commonly-occurring adverse reactions.
Phase II trials involve several hundred to a few thousand people and determine the optimum vaccine composition for achieving protection while ensuring safety.
Phase III trials involve thousands to tens of thousands of people and examine the vaccine’s ability to prevent a disease as intended. They also provide further safety information.
Post-licensure monitoring or formal Phase IV trials involve the target population. These surveillance activities identify, through spontaneous reporting systems to health authorities, less common adverse events, events which could occur after a long time, or events that may occur in specific subgroups of the target population.
Figure 11. Which other treatments, therapies, or devices are available or being evaluated? (Applied from WHO, October 2015)
CONVALESCENT BLOOD AND PLASMA
| Product / Company | Phase | Trial Location | Status |
| Convalescent plasma | Phase II/III | At MSF Ebola Treatment Centre, Donka Hospital, Conakry, Guinea
Managed by ITM Antwerp and 15 partners; funded by the European Commission and the Wellcome Trust |
As of 19 June, 101 patients were treated with convalescent plasma. |
| Convalescent plasma | Phase II/III | Liberia
Managed by ClinRM and Duke University; funded by the Bill and Melinda Gates Foundation (BMGF). |
Before Liberia was declared Ebola free on 9 May, convalescent plasma transfusions had been administered on a compassionate basis. Due to zero cases of Ebola until recently, the study in Liberia was discontinued. |
| Convalescent plasma | Phase II/III | Sierra Leone
Managed by the University of Liverpool, in collaboration with 15 other partners; funded by the Wellcome Trust and BMGF. |
As of 5 October, 3 patients have been treated with Convalescent plasma and 88 donations have been successfully collected. The first use of an apheresis machine was completed and resulted in the successful collection of 750 ml of plasma. |
Transfusion of convalescent whole blood and plasma has been prioritized for use as an investigational therapy. Convalescent whole blood donated by EVD recovered patients was currently being administered in some Ebola treatment centres in Sierra Leone. Trials using convalescent plasma are underway in Liberia and Guinea.
Assessments of national capacities for ensuring the safety of blood products outside of clinical trial settings and plans for recovery and strengthening of national blood transfusion services in the affected countries are being developed.
Figure 12. Drugs and Medicines (Applied from WHO, 2015)
Of the pre-existing medicines that were considered for re-purposing to treat Ebola, several are either being tested or considered for testing in patients with EVD or have already been used in patients with EVD. A few other therapies have also been considered for use in treatment, but have been deemed not to be appropriate for further investigation. Of the novel products, like FX06 and Zmab, some have shown initial promise in models and a few have been administered to a small number of Ebola patients on a compassionate basis. However, these cases are too few to permit any conclusion regarding safety and efficacy. Several drugs have also been used in clinical settings without prior review by WHO, including amiodarone, atorvastatin + irbesartan +/- clomiphene.
The drugs have been evaluated by the WHO Science and Technical Advisory Committee on Emergency Ebola Interventions (STAC-EE) and categorized as follows:
- Drugs already under evaluation in formal clinical trials in West Africa.
- Drugs that have been prioritized for testing in human efficacy trials, but for which such trials are not yet underway.
- Drugs that have already been given to patients for compassionate reasons or in ad hoc trials.
- Drugs that demonstrate promising anti-Ebola activity in-vitro or in mouse models, but for which additional data should be generated prior to proceeding to clinical trials.
- Drugs that had been prioritized or considered for prioritization and have now been deprioritized based on new data or more detailed analysis of old data.
| Product / Company | Phase | Trial Location | Description |
| Favipiravir
Fujifilm/Toyama, Japan |
Phase II | By INSERM in
Guinea: Conakry, Guéckedou, Macenta, Nzérékoré |
Used to treat influenza.
Clinical trials began in December 2014. Preliminary data presented in February 2015 does not permit a firm conclusion regarding efficacy and more data is required; trial continues. The drug has been administered to around 200 patients who received 9 days of oral treatment. There is no control group. The trial is at ETUs in Gueckedou, Nzerekore, Donka, and Conakry and is led by INSERM with funding from the European Commission. The EU has announced preliminary findings from these trials which show the antiviral may be effective in treating patients with early stage EVD. In adults and adolescents with a low to moderate viral load, the case fatality rate was 15% (vs 30%, historically). WHO is taking a cautious interpretation given the lack of concurrent controls in the study. |
| TKM-100802 (siRNA)
Tekmira, Canada |
Phase II | By Oxford University in
Kerry Town, Sierra Leone |
siRNA – a short RNA sequence that cleaves Ebola RNA in cells and prevents virus multiplication. Treats 100% of infected monkeys.
A clinical trial started in early March 2015 in Port Loko, Sierra Leone, led by Oxford University with funding from the Wellcome Trust. The trial was halted on 19 June on the grounds of having met one of the clinical endpoints. Continuing enrolment was not likely to demonstrate an overall therapeutic benefit. |
| ZMapp
MappBio USA |
Phase II | By NIAID in
Liberia, Sierra Leone and the United States of America |
Cocktail of three monoclonal antibodies with neutralizing activity against Ebola virus in animal models. Treats 100% of infected non-human primates (NHP). The product has been used on several patients under compassionate use.
A multi-country, multisite randomized controlled trial opened to enrollment in Liberia and the United States in February 2015 and in Sierra Leone in March 2015. Enrollment is ongoing – currently, more than 35 patients have been enrolled. No data on efficacy is available yet. Preparations to extend this trial to Guinea (in collaboration with INSERM) are in progress. |
| MIL-77
MabWorks, China |
Phase I | Cocktail of three monoclonal antibodies with the same sequence as the monoclonals in Zmapp, yet made in CHO cells.
Efficacy in monkeys comparable to Zmapp. To date, used in two expatriated patients under compassionate use. IND for Phase I filed in China. Prioritized for use on Ebola patients in condition of not interfering with the clinical assessment of efficacy of Zmapp. |
|
| BCX-4430
Biocryst, USA |
Phase I | By Quotient Clinic in the UK | Broad-spectrum direct-acting nucleoside analogue.
Phase I safety trial is underway. No efficacy trial is planned until safety data have been analysed. |
| Interferons | Phase II | By Guinea MOH in
Coyah, Guinea |
Approved for treatment of HepB and C and multiple sclerosis.
Guinean authorities, in collaboration with Canadian scientists, launched a clinical study of an interferon in Ebola-infected patients. Due to risks of symptom exacerbation, enrollment limited to patients with recent symptom onset. To date, 9 patients have been enrolled in the trial. |
| Amiodarone | Observational | At the Lakka & Goderich ETU in
Sierra Leone |
Used to treat cardiac dysrhythmia.
Was used compassionately in approximately 80 patients in Sierra Leone and reportedly reduced case fatality ratio when compared with local historical norms. The statistical significance of this result is not known due to variations in case fatality rates across sites and over time. This treatment is no longer being used. |
| Atorvostatin + Irbesartan +/- Clomiphene | Sierra Leone | Approved for cholesterol control / hypertension / infertility, respectively.
Apparently used to treat some patients in Sierra Leone, however, there has been no confirmation from the treatment centres that such studies took place, and no clinical data on the patients are available. Therefore, no conclusion on utility, safety or efficacy is possible. |
|
| FX06 | Peptide for use in treating vascular leakage.
Administered compassionately to two patients. No conclusions can be drawn yet. |
||
| Zmab | Non-GMP experimental monoclonal antibody product with no plans for GMP production.
Administered on a compassionate basis to a few patients when other products are not available. |
||
| Amodiaquine | Médecins Sans Frontiéres (MSF) | Antimalarial products were provided to all patients entering Ebola treatment centres. When MSF switched from an antimalarial containing lemefantrine to one containing amodiaquine, the case fatality rates dropped.
It is not known if this is due to efficacy of amodiaquine against Ebola or to toxicity of lemefantrine in patients with EVD. |
|
| Brincidofovir
Chimerix, USA |
Phase II | By Oxford University at the
ELWA 3 Clinic, Monrovia, Liberia |
An antiviral used to treat CMV.
Clinical trial halted and abandoned; the drug has been deprioritized for use in Ebola treatment. |
An analysis of available data from compassionate use of several therapeutic options in patients with Ebola in Europe did not lead to interpretable findings, due to polytherapy and non-standardized data collection.
WHO has also begun prioritizing the anti-malarial drug amodiaquine for testing in non-human primates. The use of this drug has been observed, in some populations, to be temporally associated with a reduction in case fatality rate. Although studies in mice show no therapeutic potential, empirical data warrant further investigation. Studies are being initiated to explore its prophylactic potential.
WHO is working with all relevant stakeholders on each of the potential therapies and vaccines to continue to accelerate identification, verification, development, and, if safety and efficacy are found, deployment.
A list of drugs that have been categorized and prioritized for consideration for testing or use in patients infected with Ebola has been published.
- Categorization and prioritization of drugs for consideration for testing or use in patients infected with Ebola
- Statement on the WHO Consultation on potential Ebola therapies and vaccines
- WHO Meeting on the Scientific and Technical Advisory Committee on Experimental Ebola Interventions – Briefing Note
Figure 13. Diagnostics (Applied from WHO, October 2015)
How is Ebola virus disease (EVD) diagnosed?
The symptoms for EVD are similar to the onset of many diseases, including influenza and malaria. The best way to diagnose whether someone with suggestive symptoms is infected with EVD is by taking a body sample, such as blood, and sending it to a laboratory that is properly equipped to handle potential Ebola specimens. In some cases, this may be a biosafety level (BSL) 3 or 4 laboratory in a neighbouring city or country. In field situations, mobile laboratories can be established in order to reduce the time between transport of the specimens and return of results. In the case of EVD, the delay caused by the need to transport specimens creates significant logistical problems with the management of potential but unconfirmed cases of EVD.
Have any new diagnostics been approved for use in the current Ebola outbreak?
| Product / Company | Description |
| RealStar® Filovirus Screen PT-PCR Kit 1.1
Altona Diagnostics GmbH, Germany |
In vitro diagnostic test that detects filovirus-specific RNA in human plasma using the QIAamp® Viral RNA Kit for RNA extraction. The assay is designed to detect all filoviruses. |
| ReEBOV Antigen Rapid Test Kit
Corgenix, USA |
This is an antigen test based on detection of the Ebola matrix protein VP40 rather than nucleic acid. |
| Liferiver™ Ebola Virus (EBOV) Real Time RT-PCR Kit
Shanghai ZJ Bio Tech Co. Ltd., China |
In vitro diagnostic test, based on real-time PCR technology intended for the detection of all highly pathogenic members of Ebolavirus: Zaire ebolavirus (ZEBOV), Sudan ebolavirus (SUDV), Taï Forest ebolavirus (TAFV) and Bundibugyo ebolavirus (BDBV) in blood, serum, plasma (non-heparin anticoagulant). |
| Xpert® Ebola Assay
Cepheid, Sweden |
The assay is a cartridge based (all reagents contained in the cartridge) that is used with the GeneXpert systems platforms that can accommodate other assays such as HIV viral load, TB, HIV qualitative and many more.
It is a real-time reverse transcription polymerase chain reaction (RT-PCR) assay but with no front end manipulation required (extraction and amplification take place in the cartridge itself) so less prone to contamination and better suited for staff without formal laboratory training. 100 times more sensitive than the benchmark assay (Altona). |
Figure 14. Knowledge about different routes of Ebola virus transmission.
| Mode of transmission | Consensus likelihood of occurring | Known | Unknown |
|---|---|---|---|
| Airborne/Aerosol (small droplet/droplet nuclei) | Unlikely from epidemiology of disease | EBOV can be aerosolized mechanically and cause lethal disease in non-human primates at low concentrations | Ability of the virus to become airborne through respiratory tract in humans and animals |
| Outbreaks contained without airborne precautions in the affected population | Airborne stability of EBOV in tropical climates | ||
| EBOV detected after 90 min in experimental small aerosols | Whether AGPs produce EBOV aerosols that cause transmission | ||
| Fomite | Less likely from environmental sampling | Virus found in dried blood | EBOV stability in tropical climates and on surfaces |
| Persists on glass and in the dark for 5.9 days | |||
| Droplet (large droplet) | Likely from epidemiology and experiments | EBOV found in stool, semen, saliva, breast milk | Whether infectious fluids are formed into droplets by humans |
| Accidental infections in non-human primates, possibly from power washing | |||
| Range of droplets containing EBOV | |||
| EBOV infections without direct contact | |||
| Bodily fluids contact | Very likely from epidemiology and experimental data | Sharing needles and handling the deceased or sick are high risk factors | How much virus is shed in different fluids |
| EBOV found in a variety of bodily fluids |
External link. Please review our privacy policy.
Figure 14. (Applied from Table 1, Judson et al, 2015)
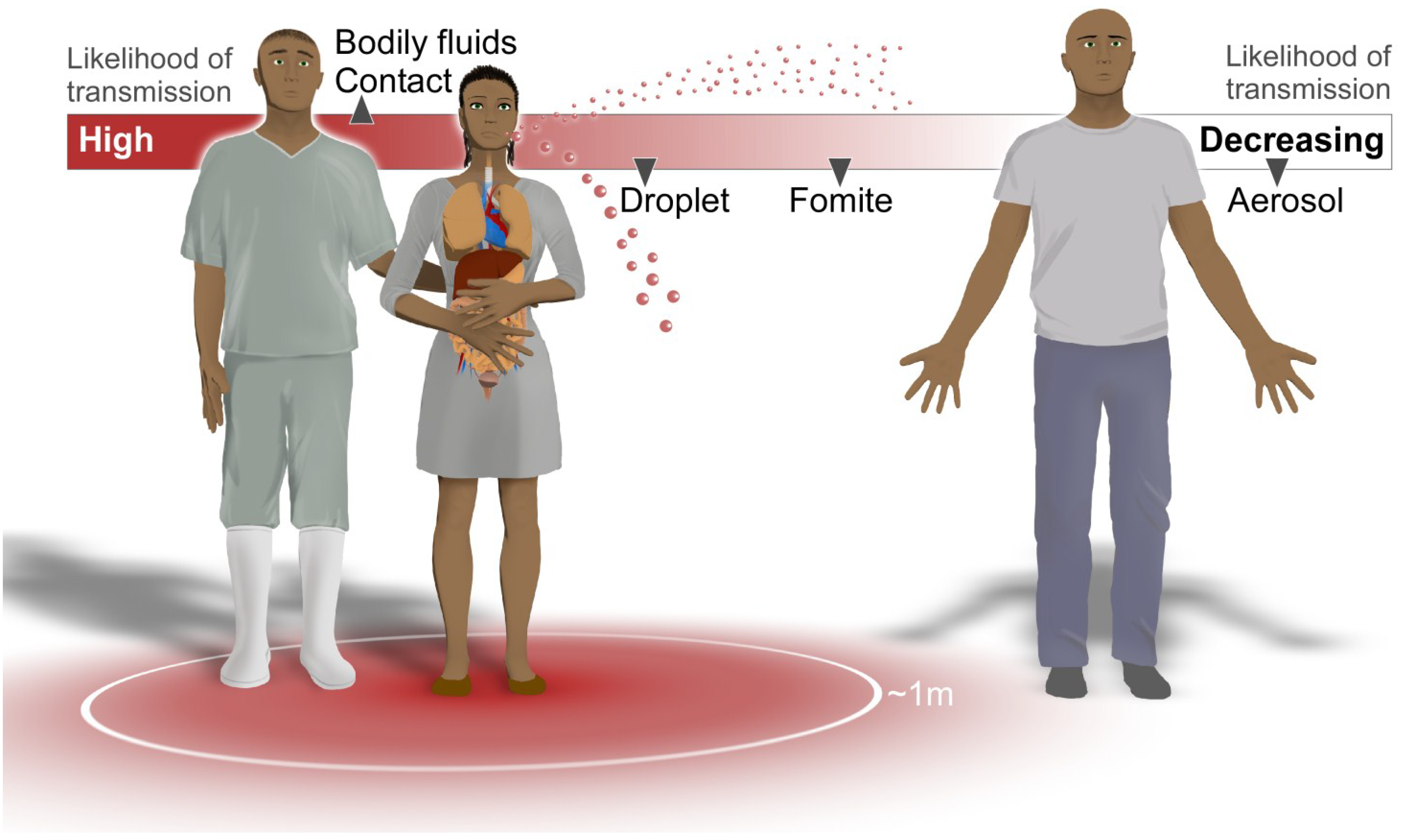
Potential Routes of Ebola Virus Transmission
Figure 15 (Applied from Figure 1, Judson et al, 2015)
Chapter 7
VII. REFERENCES
1. Bausch, D., Towner, J., Dowell, S., Kaducu, F., Lukwiya, M., Sanchez, A., Nichol, S., Ksiazek, T., Rollin, P., 2007, Assessment of the risk of Ebola virus transmission from bodily fluids and fomites. Journal of Infectious Diseases. 2007, 196 (Suppl. 2), S142–S147.
2. Carroll, S., Towner, J., Sealy, T., McMullan, L., Khristova, M., Burt, F., Swanepoel, R., Rollin, P., and Nichol, S., 2013, Molecular evolution of viruses of the family Filoviridae based on 97 whole-genome sequences, Journal of Virology. 87: 2608-2616.
3. Centers for Disease Control and Prevention, How Ebola is Spread [Pamphlet]. Atlanta. 2015.
4. Centers for Disease Control and Prevention. Outbreaks Chronology: Ebola Virus Disease 2016, http://www.cdc.gov/vhf/ebola/outbreaks/history/chronology.html
5. Darling, R., and Woods, J., 2004, Plague, USAMRIID’s Medical Management of Biological Casualties Handbook (5th ed., pp. 40-44). Fort Detrick M.D.: USAMRIID.
6. Ebolavirus, Viralzone,
http://viralzone.expasy.org/all_by_species/207.html
7.Feigin, R. D. (Ed.), 2004, Textbook of Pediatric Infectious Diseases (5th ed.). Philadelphia, USA: Elsevier, Inc.
8. Franz, D., Jahrling, P., Friedlander, A., McClain, D., Hoover, D., Bryne, W., Pavlin, J., Christopher, G., and Eitzen, E., 1997, Clinical recognition and management of patients exposed to biological warfare agents, Journal of American Medical Association, 278(5), 399-411. http://mbio.asm.org/content/6/2/e00137-15.full
9. Gire, S., Goba, A., Anderson, K., Sealfon, R., Park, D., Kanneh, L., …Sabeti, P., 2014., Genomic surveillance elucidates Ebola virus origin and transmission during the 2014 outbreak, Science, 345: 1369-1372.
10. Gupta, M., Mahanty, S., Bray, M., Ahmed, R., and Rollin, P., 2001, Passive Transfer of Antibodies Protects Immunocompetent and Immunodeficient Mice against Lethal Ebola Virus Infection without Complete Inhibition of Viral Replication, Journal of Virology, 75(10), 4649–4654. doi:10.1128/JVI.75.10.4649-4654.2001
11. Gomes, M., Piontti, A., Rossi, L., Chao, D., Longini, I., Halloran, M., Vespignani, A., Assessing the International Spreading Risk Associated with the 2014 West African Ebola Outbreak, PLOS Current Outbreaks, September 2, 2014, http://currents.plos.org/outbreaks/article/assessing-the-international-spreading-risk-associated-with-the-2014-west-african-ebola-outbreak/
12. http://evolution.berkeley.edu/evolibrary/news/141003_ebola
13. Jaax, N., Jahrling, P., Geisbert, T., Geisbert, J., Steele, K., McKee, K., Nagley, D,, Johnson, E., Jaax, G., and Peters, C., Transmission of Ebola virus (Zaire strain) to uninfected control monkeys in a biocontainment laboratory, The Lancet 346, 1669–1671 (1995).
14. Johnson, E., Jaax, N., White, J., and Jahrling, P., 1995, Lethal experimental infections of rhesus monkeys by aerosolized Ebola virus, International Journal of Pathology, 76, 227–236 (1995).
15. Judson, S., Prescott, J., and Munster, V., 2015, Understanding Ebola Virus Transmission, Viruses, 2015 Feb; 7(2): 511–521, Published online 2015 Feb 3. doi: 10.3390/v7020511
16. Kilianski A, and Evans NG, Effectively Communicating the Uncertainties Surrounding Ebola Virus Transmission, Public Library of Science Pathogens, 2015 Oct 29;11(10): e1005097. doi: 10.1371/journal.ppat.1005097. eCollection 2015.
17. Kobinger, G., Leung, A., Neufeld, J., Richardson, J., Falzarano, D., Smith, G., Tierney, K., Patel, A., and Weingartl, H., 2011, Replication, pathogenicity, shedding, and transmission of Zaire ebolavirus in pigs. Journal of Infectious Diseases, jir077.
18. Lee, J., and Saphire, E., 2009, Ebolavirus glycoprotein structure and mechanism of entry, Future Virology, 4(6), 621–635. doi:10.2217/fvl.09.56
19. Leroy, E., Kumulungui, B., Pourrut, X., Rouquet, P., Hassanin, A., Yaba, P., Délicat, A., Paweska, J., Gonzalez, J., Swanepoel, R., 2005, Fruit bats as reservoirs of Ebola virus, Nature 438, 575–576 (2005).
20. Marsh, G., Haining, J., Robinson, R., Foord, A., Yamada, M., Barr, J., Payne, J., White, J., Yu, M., Bingham, J., Rollin, P., Nichol, S., Wang, L-F., and Middleton, D., 2011, Ebola Reston virus infection of pigs: clinical significance and transmission potential, Journal of Infectious Diseases, 204 (suppl 3), S804-S809.
21. Osterholm, M., Moore, K., Kelley, N., Brosseau, L., Wong, G., Murphy, F., Peters, C., LeDuc, J., Russell, P., Van Herp, M., Kapetshi, J., Muyembe, J., Ilunga, B., Strong, J., Grolla, A., Wolz, A., Kargbo, B., Kargbo, D., Sanders, D., and Kobinger, G., 2015, Transmission of Ebola Viruses: What We Know and What We Do Not Know, doi: 10.1128/mBio.00137-15, 19 February 2015 mBio vol. 6 no. 2 e00137-15, http://mbio.asm.org/content/6/2/e00137-15.full
22. Public Health Agency of Canada, PATHOGEN SAFETY DATA SHEET – INFECTIOUS SUBSTANCES http://www.phac-aspc.gc.ca/lab-bio/res/psds-ftss/ebola-eng.php#footnote41
23. Rainisch, G., Shankar, M., Wellman, M., Merlin, T, Meltzer, M., Regional Spread of Ebola Virus, West Africa, 2014, Centers for Disease Control and Prevention, https://wwwnc.cdc.gov/eid/article/21/3/pdfs/14-1845.pdf
24. Roels, T., Bloom, A., Buffington, J., Muhungu, G., Mac Kenzie, W., Khan, A, Ndambi, R., Noah, D., Rolka, H., Peters, C., and Ksiazek T., 2010, Ebola Hemorrhagic Fever, Kikwit, Democratic Republic of the Congo, 1995: Risk Factors for Patients without a Reported Exposure, Journal of Infectious Diseases, Volume 179, Issue Supplement 1, Pp. S92-S97.
25. Sullivan, N., Yang, Z-Y, and Nabel, G., 2003, Ebola Virus Pathogenesis: Implications for Vaccines and Therapies, Journal of Virology. 2003 Sep; 77(18): 9733–9737,
doi: 10.1128/JVI.77.18.9733-9737.2003
26. Sakurai,Y., Kolokoltsov, A., Chen, C., Tidwell, M., Bauta,W., Klugbauer, N., Grimm, C., Wahl-Schott, C., Biel, M., and Davey, R., 2015, Two pore channels control Ebolavirus host cell entry and are drug targets for disease treatment, Science 347,995-998.
27. Shimojima, M., Ikeda, Y., and Kawaoka, Y., 2007,
The Mechanism of Axl-Mediated Ebola Virus Infection
Journal of Infectious Diseases. (2007) 196 (Supplement 2): S259-S263 doi:10.1086/520594
28. Shimojima, M., Takada, A., Ebihara, H., Neumann, G., Fujioka, K., Irimura, T., … Kawaoka, Y., 2006, Tyro3 Family-Mediated Cell Entry of Ebola and Marburg Viruses. Journal of Virology, 80(20), 10109–10116. doi:10.1128/JVI.01157-06
29. Spekreijse, D., Bouma, A., Koch, G., and Stegeman, A., Quantification of dust-borne transmission of highly pathogenic avian influenza virus between chickens, Influenza and Other Respiratory Viruses Volume 7, Issue 2, pages 132–138, March 2013. (Article first published online: 6 APR 2012 DOI: 10.1111/j.1750-2659.2012.00362.x)
30. Tang, J., Li, Y., Eames, I., Chan, P., Ridgway, G., 2006, Factors involved in the aerosol transmission of infection and control of ventilation in healthcare premises, Journal of Hospital Infection. 2006, 64, 100–114.
31. Tellier, R. Aerosol transmission of influenza A virus: A review of new studies, Journal of Royal Society Interface 2009, 6 (Suppl. 6), S783–S790.
32. WHO, Ebola virus disease, Fact sheet No 103, Updated January 2016, http://www.who.int/mediacentre/factsheets/fs103/en/
33. Weingartl, H., Embury-Hyatt, C., Nfon, C., Leung, A., Smith, G., and Kobinger,G., 2012, Transmission of Ebola virus from pigs to non-human primates, Nature, November, 2012, http://www.nature.com/articles/srep00811
34. Weissenhorn, W., Calder, L., Wharton, S., Skehel,J., and Wiley, D., 1998, The central structural feature of the membrane fusion protein subunit from the Ebola virus glycoprotein is a long triple-stranded coiled coil, Proceedings of the National Academy of Sciences of the United States of America, 1998 May 26; 95(11): 6032–6036, PMCID: PMC27580

